Perineal nerve palsy is a condition that can cause significant discomfort and disruption in daily life. It is crucial to have a clear understanding of the causes, symptoms, and treatment options to effectively manage and cope with this condition. In this article, we will delve deeper into what perineal nerve palsy is, explore its causes, discuss the various symptoms that may arise, highlight diagnostic procedures, and finally, provide an overview of the available treatment options.
What is Perineal Nerve Palsy?
Perineal nerve palsy refers to the dysfunction or damage of the perineal nerve, which is responsible for supplying the sensation and motor control to the perineal region. The perineum is the area located between the genitals and the anus. When this nerve is affected, individuals may experience a range of symptoms that can significantly impact their quality of life.
Defining Perineal Nerve Palsy
The perineal nerve, also known as the pudendal nerve, originates from the sacral plexus and consists of several branches that innervate the pelvic and perineal regions. When there is damage or injury to this nerve, it can result in perineal nerve palsy, leading to various complications.
The Anatomy of the Perineal Nerve
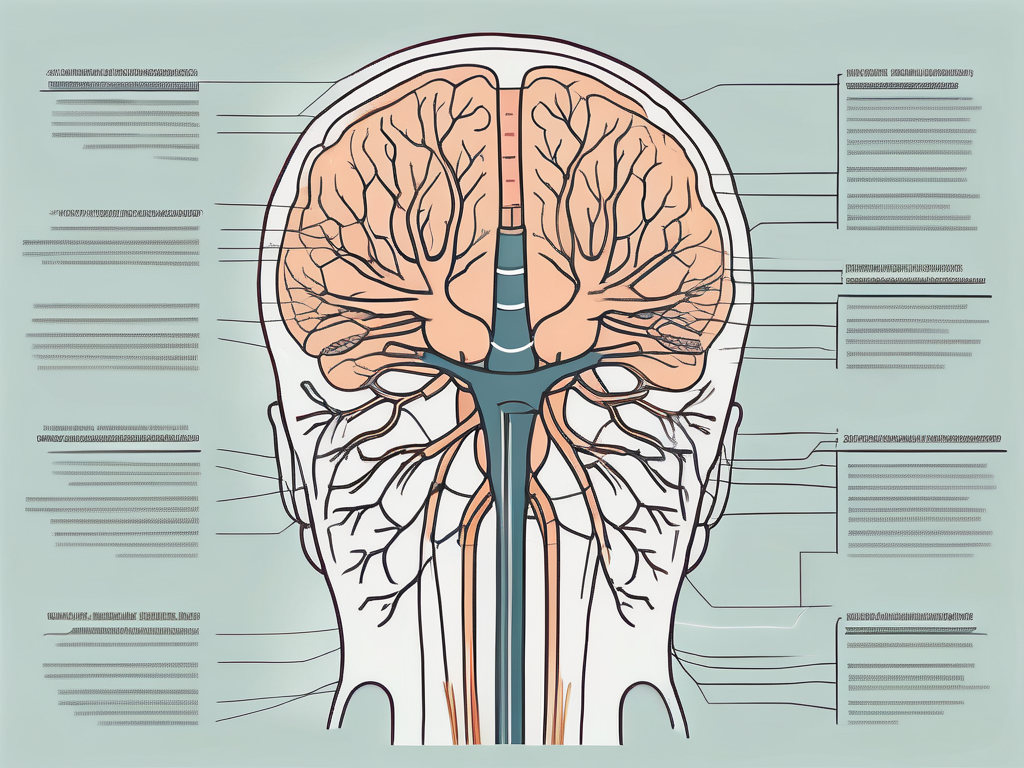
To understand perineal nerve palsy fully, it is essential to have a basic understanding of the anatomy of the perineal nerve. The perineal nerve originates from the sacral plexus, which is a network of nerves in the lower back. It travels through the pelvis, eventually reaching the perineum. This nerve provides sensation to the genitals, perineal area, and anal region while also controlling the muscles in these regions.
The perineal nerve is a crucial component of the peripheral nervous system, playing a vital role in maintaining the normal function of the perineal region. It is responsible for transmitting sensory information from the perineum to the brain, allowing individuals to perceive touch, pressure, and temperature in this area. Additionally, the perineal nerve controls the contraction and relaxation of the muscles in the perineum, enabling voluntary control over urination, defecation, and sexual function.
When perineal nerve palsy occurs, it can disrupt the normal functioning of the perineum, leading to a variety of symptoms. These symptoms may include numbness or tingling in the perineal area, decreased sensation during sexual activity, difficulty controlling bowel or bladder movements, and weakness or paralysis of the muscles in the perineum. The severity of these symptoms can vary depending on the extent of nerve damage and the underlying cause of perineal nerve palsy.
Perineal nerve palsy can be caused by various factors, including trauma or injury to the perineum, compression of the nerve due to prolonged sitting or cycling, childbirth-related injuries, pelvic surgery, or underlying medical conditions such as diabetes or multiple sclerosis. Proper diagnosis and treatment of perineal nerve palsy are essential to alleviate symptoms and improve the individual’s quality of life.
Treatment options for perineal nerve palsy may include conservative measures such as pain management, physical therapy, and lifestyle modifications. In some cases, surgical intervention may be necessary to repair or decompress the affected nerve. The specific treatment approach will depend on the underlying cause and severity of the condition.
In conclusion, perineal nerve palsy is a condition characterized by dysfunction or damage to the perineal nerve, leading to a range of symptoms that can significantly impact an individual’s quality of life. Understanding the anatomy and function of the perineal nerve is crucial in diagnosing and treating this condition effectively. With proper medical intervention and management, individuals with perineal nerve palsy can experience improved symptom control and regain their normal daily activities.
Causes of Perineal Nerve Palsy
Medical Conditions Leading to Perineal Nerve Palsy
There are several medical conditions that can contribute to the development of perineal nerve palsy. Some common causes include trauma during childbirth, prolonged sitting or cycling, pelvic surgery, chronic constipation, and certain diseases such as diabetes, multiple sclerosis, or pelvic tumors. It is important to note that perineal nerve palsy can occur due to a combination of factors, and each individual case may vary.
One of the medical conditions that can lead to perineal nerve palsy is trauma during childbirth. The pressure exerted on the perineum during delivery can cause damage to the nerves in the area, resulting in palsy. This can be a temporary condition that resolves on its own over time, or it can be a more severe and long-lasting condition that requires medical intervention.
Prolonged sitting or cycling can also contribute to the development of perineal nerve palsy. When individuals spend long periods of time in a seated position, especially on hard surfaces, the constant pressure on the perineal region can lead to nerve damage. Similarly, the repetitive motion and pressure exerted on the perineum during cycling can also cause palsy over time.
Pelvic surgery is another potential cause of perineal nerve palsy. During surgical procedures that involve the pelvic area, there is a risk of damaging the perineal nerves. This can occur due to accidental injury during the surgery or as a result of the surgical instruments putting pressure on the nerves.
Chronic constipation, a condition characterized by infrequent bowel movements and difficulty passing stool, can also contribute to the development of perineal nerve palsy. The straining and pressure exerted during bowel movements can put stress on the perineal region, potentially leading to nerve damage over time.
Furthermore, certain diseases can increase the risk of perineal nerve palsy. Diabetes, for example, can cause nerve damage throughout the body, including the perineal nerves. Multiple sclerosis, a chronic autoimmune disease that affects the central nervous system, can also lead to nerve dysfunction, potentially resulting in palsy. Additionally, pelvic tumors can put pressure on the perineal nerves, causing damage and subsequent palsy.
Injuries Resulting in Perineal Nerve Palsy
Injuries or trauma to the perineal region can also lead to perineal nerve palsy. Accidents involving direct impact to the pelvic area or surgeries that involve the perineum may cause damage to the nerve. For example, a fall or a sports-related injury that directly affects the perineum can result in palsy.
Additionally, prolonged pressure or compression on the perineal region, such as in individuals who spend long periods sitting on hard surfaces, can also lead to this condition. Occupations that require prolonged sitting, such as truck driving or desk jobs, can increase the risk of developing perineal nerve palsy. The constant pressure on the perineum restricts blood flow and can cause nerve damage over time.
In conclusion, perineal nerve palsy can be caused by various medical conditions and injuries. Understanding the potential causes can help individuals take preventive measures and seek appropriate medical care when necessary. It is important to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
Recognizing the Symptoms of Perineal Nerve Palsy
Perineal nerve palsy is a condition that can cause a range of physical and sensory symptoms. It occurs when the perineal nerve, which is responsible for providing sensation to the genital area, perineum, and anal region, becomes damaged or compressed. The symptoms of perineal nerve palsy can vary from individual to individual, but there are some common physical and sensory symptoms that may be experienced.
Physical Symptoms
The physical symptoms of perineal nerve palsy can be distressing and can greatly impact an individual’s daily life. One of the most common physical symptoms is a loss of sensation or numbness in the affected area. This can make it difficult for individuals to feel touch or pain in the genital area, perineum, and anal region. It can also lead to difficulties with bowel movements and urination, as the loss of sensation can make it challenging to control these bodily functions.
In addition to the loss of sensation, some individuals may also experience weakness in the pelvic floor muscles. The pelvic floor muscles play a crucial role in supporting the organs in the pelvic region, and weakness in these muscles can lead to problems such as urinary incontinence or pelvic organ prolapse. These physical symptoms can have a significant impact on an individual’s quality of life and may require medical intervention to manage.
Sensory Symptoms
Alongside the physical symptoms, individuals with perineal nerve palsy may also experience sensory symptoms. These sensory symptoms can vary in intensity and can greatly affect an individual’s comfort and well-being. One common sensory symptom is a tingling or “pins and needles” sensation in the affected area. This sensation can be uncomfortable and may persist for extended periods of time.
In addition to the tingling sensation, some individuals may also experience burning or shooting pain in the affected region. This pain can be sharp and intense, making it difficult for individuals to engage in regular activities or find relief. The sensory symptoms associated with perineal nerve palsy can greatly impact an individual’s quality of life, causing discomfort and even interfering with their ability to carry out daily activities.
It is important to recognize the symptoms of perineal nerve palsy and seek medical attention if you suspect you may be experiencing this condition. Early diagnosis and treatment can help manage the symptoms and improve the individual’s overall well-being. If you are experiencing any of the physical or sensory symptoms mentioned, it is advisable to consult with a healthcare professional for a proper evaluation and guidance on the best course of action.
Diagnostic Procedures for Perineal Nerve Palsy
Medical History and Physical Examination
Diagnosing perineal nerve palsy typically begins with a comprehensive medical history and physical examination. The healthcare provider will inquire about the individual’s symptoms, medical history, and any potential risk factors. A physical examination may involve assessing the sensation, muscle strength, and reflexes in the affected area. This initial evaluation helps healthcare professionals determine the need for further testing.
During the medical history assessment, the healthcare provider will ask specific questions to gather information about the onset, duration, and progression of symptoms. They will also inquire about any previous injuries or surgeries that may have affected the perineal region. Additionally, the healthcare provider will explore potential risk factors such as diabetes, obesity, or prolonged sitting or cycling habits, which can contribute to the development of perineal nerve palsy.
During the physical examination, the healthcare provider will carefully examine the perineal region. They will assess the sensation by using a variety of techniques such as light touch, pinprick, or temperature sensation tests. Muscle strength will be evaluated by asking the individual to perform specific movements or resist against the healthcare provider’s resistance. Reflexes in the affected area, such as the anal wink reflex, may also be tested to assess the integrity of the perineal nerve.
Imaging and Neurological Tests
Once an initial assessment is completed, further diagnostic tests may be required to confirm the diagnosis of perineal nerve palsy and rule out other potential causes. Imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can help visualize the perineal region and identify any structural abnormalities or nerve compression.
MRI uses a powerful magnetic field and radio waves to create detailed images of the internal structures of the body. It can provide a clear view of the perineal region, allowing healthcare professionals to identify any potential nerve damage, tumors, or other abnormalities that may be causing the symptoms of perineal nerve palsy. CT scans, on the other hand, use a series of X-ray images taken from different angles to create cross-sectional images of the body. This imaging technique can also help visualize the perineal region and provide valuable information about the underlying cause of the nerve palsy.
In addition to imaging tests, neurological tests such as electromyography (EMG) may be conducted to assess nerve conduction and muscle function. During an EMG, small electrodes are inserted into the muscles of the perineal region to measure the electrical activity. This test can help determine the extent of nerve damage and identify the specific muscles affected by the perineal nerve palsy.
Overall, the combination of medical history assessment, physical examination, imaging tests, and neurological tests allows healthcare professionals to accurately diagnose perineal nerve palsy and develop an appropriate treatment plan. Early diagnosis and intervention can significantly improve the prognosis and quality of life for individuals with this condition.
Treatment Options for Perineal Nerve Palsy
Non-Surgical Treatments
In many cases, non-surgical treatments can effectively manage the symptoms associated with perineal nerve palsy. These may include pain management techniques, such as medication or physical therapy, to alleviate discomfort and improve functionality. Lifestyle adjustments, such as avoiding prolonged sitting or pressure on the perineal region, may also be beneficial. In some instances, pelvic floor exercises or biofeedback therapy may be recommended to strengthen the pelvic muscles and improve bladder and bowel control.
Physical therapy is a commonly used non-surgical treatment for perineal nerve palsy. This therapy involves exercises and stretches that target the affected muscles and nerves. The goal is to improve range of motion, reduce pain, and increase strength. A physical therapist will work closely with the patient to develop a personalized treatment plan that addresses their specific needs and goals.
Another non-surgical treatment option is medication. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, may be prescribed to manage pain associated with perineal nerve palsy. These medications can help reduce inflammation and alleviate discomfort. Additionally, nerve pain medications, such as gabapentin or pregabalin, may be prescribed to target the specific nerve-related symptoms.
Lifestyle adjustments can also play a significant role in managing perineal nerve palsy. Avoiding activities that put pressure on the perineal region, such as sitting for long periods or cycling, can help reduce symptoms. Using cushions or padded seats can provide additional support and alleviate pressure. It is important to maintain good posture and take frequent breaks to avoid prolonged pressure on the affected area.
In some cases, pelvic floor exercises or biofeedback therapy may be recommended as part of the non-surgical treatment plan. Pelvic floor exercises, also known as Kegel exercises, involve contracting and relaxing the muscles of the pelvic floor. These exercises can help strengthen the muscles and improve bladder and bowel control. Biofeedback therapy uses sensors to provide feedback on muscle activity, helping patients learn how to control and strengthen their pelvic floor muscles.
Surgical Interventions
In more severe cases or when conservative treatments do not provide sufficient relief, surgical interventions may be considered. The specific surgical procedure will depend on the underlying cause of perineal nerve palsy. Surgical options may include nerve decompression or repair, removal of any compressing structures, or reconstructive procedures to improve nerve function. It is important to consult with a healthcare professional to determine the most suitable surgical approach based on individual circumstances.
Nerve decompression is a surgical procedure that involves relieving pressure on the affected nerve. This can be achieved by removing any surrounding tissue or structures that may be compressing the nerve. By alleviating the pressure, the nerve can function more effectively, reducing symptoms and improving overall function.
In cases where there is significant nerve damage, nerve repair may be necessary. This involves surgically reconnecting or grafting the damaged nerve to restore its function. The success of nerve repair surgery depends on various factors, including the extent of the damage and the individual’s overall health.
Reconstructive procedures may be considered in cases where there is extensive nerve damage or loss. These procedures aim to restore function and improve quality of life. Options may include nerve transfers, where a healthy nerve is redirected to replace the damaged one, or nerve grafts, where a section of nerve is taken from another part of the body and used to repair the damaged nerve.
It is important to note that surgical interventions carry risks and potential complications. These should be thoroughly discussed with a healthcare professional, who can provide detailed information and guidance based on the individual’s specific condition and needs.
Living with Perineal Nerve Palsy
Coping Mechanisms and Lifestyle Adjustments
Living with perineal nerve palsy can present unique challenges. However, there are coping mechanisms and lifestyle adjustments that can assist individuals in managing their symptoms and improving their quality of life. Engaging in relaxation techniques, such as meditation or yoga, can help alleviate stress and reduce pain levels. Exploring pain management strategies, such as acupuncture or transcutaneous electrical nerve stimulation (TENS), may also provide relief.
Support and Resources for Patients
It is essential for individuals with perineal nerve palsy to seek support and resources that can assist in their journey. Connecting with support groups or online communities comprised of individuals facing similar challenges can provide valuable emotional support and information sharing. Additionally, seeking guidance from healthcare professionals, such as physical therapists or pain management specialists, can help individuals navigate their treatment options and obtain personalized care.
In summary, perineal nerve palsy is a condition that can significantly impact an individual’s well-being. Understanding the causes, recognizing the symptoms, and exploring available treatment options are crucial steps towards effectively managing and coping with this condition. It is important for individuals experiencing symptoms of perineal nerve palsy to consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan tailored to their specific needs. With proper care and support, individuals can regain control over their lives and improve their overall quality of life.