Perineal nerve damage is a condition that can have a significant impact on a person’s daily life. It can cause physical symptoms, emotional and psychological distress, and may significantly affect one’s mobility and personal relationships. Recognizing the symptoms and understanding the causes of perineal nerve damage is crucial for early detection and effective treatment. In this article, we will explore the various aspects of perineal nerve damage, including its anatomy, common causes, symptoms, diagnostic procedures, treatment options, prevention strategies, and tips for living with this condition.
What is Perineal Nerve Damage?
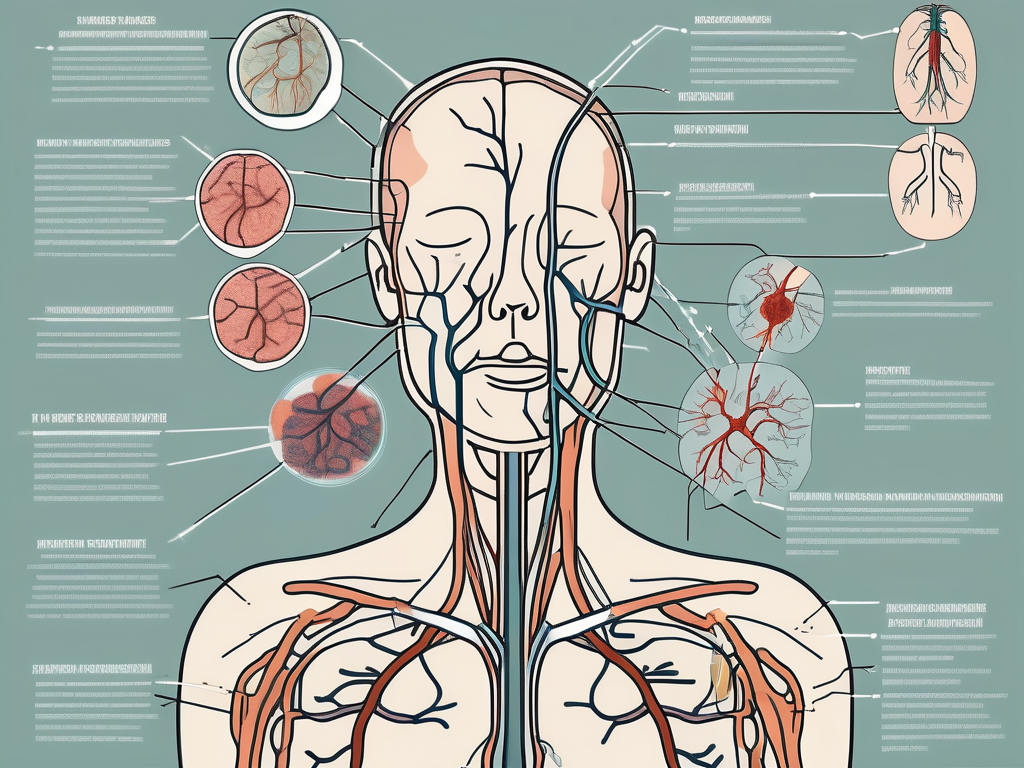
Perineal nerve damage refers to any injury or impairment to the perineal nerve, which is a branch of the pudendal nerve located in the pelvic region. The perineal nerve supplies sensation to the perineum, a region between the anus and external genitalia, as well as the lower part of the rectum, the scrotum in males, and the labia majora in females. Damage to this nerve can lead to a variety of symptoms and complications.
Anatomy of the Perineal Nerve
The perineal nerve is a mixed nerve composed of sensory and motor fibers. It originates from the second, third, and fourth sacral nerve roots and travels through the pelvis before branching into various smaller nerves. These nerves innervate the muscles and skin of the perineal region. Understanding the anatomy of the perineal nerve helps in grasping the potential consequences of damage to this vital nerve.
The perineal nerve is an essential component of the peripheral nervous system, responsible for transmitting signals between the brain and the perineal region. It plays a crucial role in maintaining normal sensation and function in the area. The sensory fibers of the perineal nerve allow individuals to perceive touch, pain, and temperature in the perineum, while the motor fibers enable the contraction and relaxation of the muscles in the region.
Furthermore, the perineal nerve communicates with other nerves in the pelvic region, forming a complex network that ensures coordinated movement and sensation. This intricate network allows for normal bladder and bowel function, sexual function, and overall comfort in daily activities.
Common Causes of Perineal Nerve Damage
Perineal nerve damage can occur due to a range of factors, including trauma, compression, inflammation, and disease. Traumatic injuries, such as pelvic fractures or childbirth-related injuries, can damage the nerve directly or indirectly. The perineal nerve may be stretched, compressed, or torn during accidents or difficult deliveries, leading to varying degrees of nerve damage.
Prolonged pressure on the nerve, as seen in individuals who spend long hours sitting, can also lead to nerve damage. Occupations that require prolonged sitting, such as truck driving or office work, may increase the risk of developing perineal nerve damage. The constant pressure on the nerve can impede blood flow and cause nerve compression, resulting in symptoms such as numbness, tingling, or pain in the perineal region.
Additionally, certain medical conditions can increase the risk of perineal nerve damage. Diabetes, for example, can cause nerve damage throughout the body, including the perineal nerve. The high blood sugar levels associated with diabetes can lead to nerve dysfunction and impaired sensation in the perineal region. Infections, such as sexually transmitted infections or urinary tract infections, can also cause inflammation and damage to the perineal nerve. Autoimmune disorders, where the immune system mistakenly attacks the body’s own tissues, can also affect the perineal nerve.
It is important to note that each case of perineal nerve damage is unique, and the underlying cause may vary for different individuals. Proper diagnosis and treatment are essential for managing the symptoms and preventing further complications.
Recognizing the Symptoms of Perineal Nerve Damage
Perineal nerve damage can manifest through various physical symptoms and may also have a profound impact on one’s emotional and psychological well-being. Understanding and recognizing these symptoms is crucial for early diagnosis and effective management of this condition.
Physical Symptoms
Common physical symptoms associated with perineal nerve damage include:
- Numbness or tingling in the perineal region: This sensation can be unsettling and may affect daily activities such as sitting or walking.
- Pain or discomfort during urination or bowel movements: The perineal area plays a crucial role in these bodily functions, and any damage to the nerve can lead to pain or discomfort.
- Reduced sensitivity during sexual activity: Perineal nerve damage can impact sexual function and pleasure, causing frustration and affecting intimate relationships.
- Muscle weakness in the pelvic area: The perineal nerve is responsible for controlling the muscles in the pelvic region. Weakness in these muscles can lead to difficulties with bladder and bowel control.
Experiencing these physical symptoms can significantly affect an individual’s quality of life. It is important to seek medical attention for proper diagnosis and management of perineal nerve damage.
Emotional and Psychological Symptoms
Dealing with perineal nerve damage can be emotionally challenging. In addition to the physical limitations, individuals may experience a range of emotional and psychological symptoms:
- Frustration: Coping with the physical symptoms and limitations can be frustrating, especially when they interfere with daily activities and personal relationships.
- Anxiety: The uncertainty surrounding the condition and its potential long-term effects can lead to anxiety and worry.
- Depression: Chronic pain and the impact on daily life can contribute to feelings of sadness and depression.
- Decreased self-esteem: Changes in sexual function and the physical appearance of the perineal region may lead to a decreased sense of self-esteem and body image issues.
Addressing these emotional aspects is vital for comprehensive care and overall well-being. Support from healthcare professionals, therapists, and support groups can help individuals navigate the emotional challenges associated with perineal nerve damage.
It is important to remember that every individual’s experience with perineal nerve damage may vary. Seeking professional medical advice and personalized care is essential for proper diagnosis, treatment, and support.
The Impact of Perineal Nerve Damage on Daily Life
Perineal nerve damage can have a profound impact on various aspects of daily life, including mobility and personal relationships.
Perineal nerve damage is a condition that can occur due to various factors such as trauma, surgery, or medical conditions. When the perineal nerve, which plays a crucial role in innervating the pelvic muscles, is damaged, it can result in compromised mobility and affect personal relationships.
Impact on Mobility
Because the perineal nerve plays a crucial role in innervating the pelvic muscles, damage to this nerve can result in compromised mobility. Individuals may experience difficulties in walking, maintaining balance, or controlling their bladder or bowel movements.
Walking, a seemingly simple task for most people, can become a challenge for those with perineal nerve damage. The loss of proper muscle function in the pelvic area can affect the stability and coordination required for walking. Individuals may find themselves relying on assistive devices such as canes or walkers to maintain their balance and prevent falls.
In addition to walking difficulties, perineal nerve damage can also impact an individual’s ability to control their bladder and bowel movements. The loss of nerve function can lead to urinary or fecal incontinence, which can be embarrassing and affect one’s confidence and independence. Occupational and physical therapy, as well as assistive devices, can help individuals regain mobility and independence.
Impact on Personal Relationships
Perineal nerve damage can also affect personal relationships, particularly those of a sexual nature. The loss of sensation or pain during sexual activity can lead to challenges in intimate relationships.
Sexual intimacy is an important aspect of many relationships, and perineal nerve damage can significantly impact this area of life. The loss of sensation in the pelvic region can make sexual activity less pleasurable or even painful. This can lead to frustration, decreased sexual desire, and emotional strain on both partners.
Open communication between partners is crucial in navigating the challenges posed by perineal nerve damage. Discussing concerns, fears, and exploring alternative means of sexual intimacy can help maintain a healthy and fulfilling relationship. Couples may need to explore different sexual techniques, use lubricants or other aids, or seek the guidance of healthcare professionals specializing in sexual health.
It is important to remember that perineal nerve damage does not define a person’s worth or their ability to have fulfilling relationships. With support, understanding, and the right resources, individuals with perineal nerve damage can adapt to the challenges they face and continue to lead fulfilling lives.
Diagnostic Procedures for Perineal Nerve Damage
Recognizing the symptoms of perineal nerve damage and identifying its underlying causes requires a comprehensive diagnostic approach. Perineal nerve damage can cause a variety of symptoms, including numbness, tingling, pain, and weakness in the perineal region. These symptoms can greatly affect a person’s quality of life and may require medical intervention.
When a patient presents with symptoms suggestive of perineal nerve damage, medical professionals employ various diagnostic procedures to determine the extent of the damage and its underlying cause. These procedures aim to provide a thorough understanding of the patient’s condition and guide appropriate treatment strategies.
Medical History and Physical Examination
An essential component of the diagnostic process is a detailed medical history and a thorough physical examination. Medical professionals will inquire about symptoms, previous medical conditions, and potential risk factors. Gathering this information helps in identifying any potential causes or contributing factors to the perineal nerve damage.
The physical examination may involve sensory and strength testing in the perineal region. By assessing the patient’s responses to different stimuli, medical professionals can gain insights into the specific nerves affected and the severity of the damage. Additionally, reflexes in the perineal area may be tested to further evaluate the nerve function.
Imaging and Laboratory Tests
To further evaluate the extent of nerve damage and determine the underlying cause, medical imaging tests like MRI scans or nerve conduction studies might be recommended. These tests provide detailed images of the perineal region, allowing medical professionals to visualize any structural abnormalities or compression on the nerves.
Nerve conduction studies, on the other hand, measure the speed and strength of electrical signals as they travel along the nerves. This test can help identify the location and severity of nerve damage, aiding in the diagnosis and treatment planning.
Additionally, blood tests may be conducted to identify any infections or systemic conditions that could be contributing to the nerve damage. These tests can detect markers of inflammation, autoimmune disorders, or infections that may be affecting the perineal nerves.
Overall, the diagnostic procedures for perineal nerve damage involve a comprehensive assessment of the patient’s medical history, physical examination, and additional imaging or laboratory tests. By combining these approaches, medical professionals can accurately diagnose the condition and develop an appropriate treatment plan tailored to the individual patient’s needs.
Treatment Options for Perineal Nerve Damage
The treatment approach for perineal nerve damage depends on the underlying cause, severity of symptoms, and individual circumstances. Perineal nerve damage can result from various factors, such as trauma, compression, or disease. It can lead to symptoms like pain, numbness, tingling, and loss of function in the perineal region.
When it comes to treating perineal nerve damage, healthcare professionals consider both non-surgical and surgical options. The choice of treatment depends on the specific needs and condition of the patient.
Non-Surgical Treatments
Non-surgical treatments focus on symptom management and rehabilitation. Pain management techniques play a crucial role in alleviating discomfort and improving function. Healthcare professionals may prescribe medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or neuropathic pain medications, to help manage pain associated with perineal nerve damage.
In addition to medication, physical therapy can be an effective non-surgical treatment option. Physical therapists can design personalized exercise programs to strengthen the muscles surrounding the perineal region and improve overall function. They may also incorporate techniques like manual therapy and stretching to reduce muscle tension and improve flexibility.
Nerve stimulation is another non-surgical approach that can be beneficial for individuals with perineal nerve damage. Techniques such as transcutaneous electrical nerve stimulation (TENS) or percutaneous electrical nerve stimulation (PENS) can help reduce pain and improve nerve function.
Lifestyle modifications are also important in managing perineal nerve damage. Healthcare professionals may recommend appropriate exercise routines, such as pelvic floor exercises, to strengthen the muscles in the perineal region. Maintaining a healthy weight is crucial, as excess weight can put additional pressure on the nerves. Furthermore, avoiding activities or positions that cause excessive pressure on the perineal area can help prevent further damage.
It is essential for individuals with perineal nerve damage to work closely with healthcare professionals to develop a personalized treatment plan. Regular follow-ups and adjustments to the treatment approach may be necessary to ensure optimal outcomes.
Surgical Treatments
In some cases, surgical intervention may be necessary to address the underlying cause or relieve pressure on the perineal nerve. Surgical options for perineal nerve damage are tailored to the individual’s specific needs and condition.
One surgical option is decompression of nerve impingement. This procedure involves relieving pressure on the perineal nerve by removing or adjusting the structures that are compressing it. By doing so, the nerve can regain its normal function, and symptoms can be alleviated.
In cases where the perineal nerve has been severely damaged or severed, nerve grafting may be considered. Nerve grafting involves taking a healthy nerve from another part of the body and using it to bridge the gap in the damaged nerve. This procedure aims to restore nerve function and improve symptoms.
It is important to note that the decision to undergo surgery should be made in consultation with a qualified healthcare professional. They will assess the individual’s condition, discuss the potential risks and benefits of surgery, and provide guidance on the most appropriate course of action.
In conclusion, treatment options for perineal nerve damage range from non-surgical approaches focused on symptom management and rehabilitation to surgical interventions aimed at addressing the underlying cause or relieving pressure on the nerve. The choice of treatment depends on various factors, and a personalized approach is crucial for optimal outcomes.
Prevention Strategies for Perineal Nerve Damage
While not all cases of perineal nerve damage can be prevented, there are strategies individuals can adopt to minimize the risk and promote overall nerve health.
Lifestyle Modifications
Engaging in regular exercise, maintaining a healthy weight, and adopting proper ergonomics and body mechanics can help reduce the risk of trauma or compression on the perineal nerve. It is also important to prioritize breaks and posture adjustments during activities that involve prolonged sitting or pressure on the perineal region.
Regular Check-ups and Early Detection
Regular medical check-ups and discussions with healthcare professionals are essential for the early detection of any signs or symptoms of perineal nerve damage. Early detection can facilitate timely intervention and prompt management, potentially minimizing the long-term impact of the condition.
Living with Perineal Nerve Damage
Coping Mechanisms and Support Systems
Living with perineal nerve damage can be challenging, both physically and emotionally. Coping mechanisms, such as seeking support from loved ones, joining support groups, practicing relaxation techniques, and engaging in activities that bring joy, can contribute to overall well-being. Professional counseling or therapy may also provide valuable support in navigating the emotional aspects of living with this condition.
Long-Term Management and Prognosis
Perineal nerve damage is a chronic condition that may require ongoing management. Each individual’s prognosis and long-term outcomes may vary depending on the underlying cause, severity of nerve damage, and response to treatment. It is crucial to maintain open communication with healthcare professionals, follow recommended treatment plans, and attend regular follow-up appointments to ensure appropriate management and to address any new or worsening symptoms.
While this article provides an in-depth understanding of perineal nerve damage, it is important to consult with a healthcare professional for accurate diagnosis, tailored treatment plans, and any specific medical advice. The information presented in this article is based on general knowledge and should not replace individualized medical guidance.