The perineal nerve is a crucial component of the human anatomy, playing a significant role in various bodily functions. As such, having a comprehensive understanding of its structure, functions, disorders, and treatment options is essential. In this guide, we will delve into the intricacies of perineal nerve anatomy, explore its importance, discuss related disorders, and provide insights into prevention and management strategies. Additionally, we will highlight future research directions in perineal nerve health, including emerging treatments and the potential role of technology.
Introduction to Perineal Nerve Anatomy
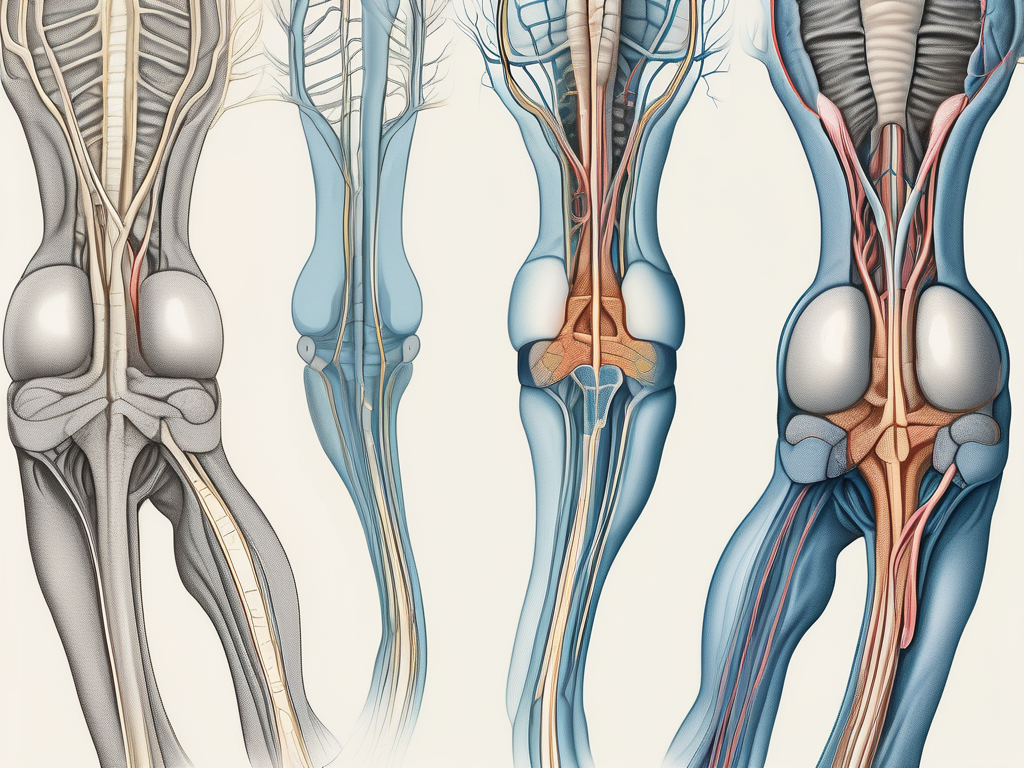
The perineal nerve, a branch of the pudendal nerve, is a critical component of the sacral plexus. It originates from the S2 to S4 nerve roots and innervates the perineum, a region located between the pubic symphysis and the coccyx. This complex network of nerves plays a pivotal role in both motor and sensory functions.
The perineal nerve is named after the perineum, which is a diamond-shaped area between the thighs that includes the external genitalia and the anus. This region is rich in nerve endings and is responsible for various sensations and functions.
Understanding the anatomy of the perineal nerve is crucial for medical professionals, as it is involved in many important bodily functions and can be affected by various conditions.
The Importance of the Perineal Nerve
The perineal nerve is vital for maintaining normal bladder, bowel, and sexual functions. It supplies sensory fibers to the perineal region, external genitalia, and anal canal, allowing for the perception of touch, pressure, and temperature. This sensory input is essential for sexual arousal and pleasure, as well as for the proper functioning of the urinary and digestive systems.
In addition to its sensory role, the perineal nerve also facilitates the contraction of muscles involved in urinary and fecal control, ensuring appropriate continence. The motor fibers of the perineal nerve innervate the muscles of the perineum, including the anal sphincter and bulbospongiosus muscle. These muscles play a crucial role in maintaining continence and are responsible for controlling the release of urine and feces.
Damage or dysfunction of the perineal nerve can lead to various problems, such as urinary and fecal incontinence, sexual dysfunction, and loss of sensation in the perineal region. Therefore, understanding the anatomy and function of this nerve is essential for diagnosing and treating these conditions.
Basic Structure of the Perineal Nerve
The perineal nerve follows a distinct anatomical pathway, branching into several divisions. As it courses through the pelvis, it gives rise to sensory and motor branches that supply various structures.
The sensory components of the perineal nerve originate from the dorsal nerve of the penis or clitoris, depending on the gender. These branches provide sensory innervation to the external genitalia, including the penis or clitoris, labia, and surrounding skin. They also supply the anal canal, allowing for the perception of touch, pressure, and temperature in these areas.
On the other hand, the motor fibers of the perineal nerve innervate the muscles of the perineum. These include the anal sphincter, which is responsible for controlling the release of feces, and the bulbospongiosus muscle, which plays a role in sexual function. The motor branches of the perineal nerve ensure the proper functioning of these muscles, allowing for voluntary control of urination, defecation, and sexual activities.
In summary, the perineal nerve is a crucial component of the sacral plexus, responsible for maintaining normal bladder, bowel, and sexual functions. Its sensory branches provide perception to the perineal region and external genitalia, while its motor branches innervate the muscles involved in urinary and fecal control. Understanding the anatomy and function of the perineal nerve is essential for healthcare professionals in diagnosing and treating conditions related to this important nerve.
Detailed Overview of the Perineal Nerve
Let’s explore the perineal nerve in more detail, examining its branches and functions.
The perineal nerve is a crucial component of the peripheral nervous system, playing a vital role in the innervation and function of various structures in the perineal region. It originates from the sacral plexus, a complex network of nerves located in the lower back.
Branches of the Perineal Nerve
The perineal nerve gives rise to several important branches, each with its own unique role in ensuring the proper function of specific structures.
Inferior Rectal Nerve: One of the branches of the perineal nerve is the inferior rectal nerve. This branch provides sensory innervation to the anal canal, perianal skin, and the external anal sphincter. It plays a crucial role in the perception of touch, pain, and temperature in the anal region.
Dorsal Nerve of the Penis or Clitoris: Another significant branch of the perineal nerve is the dorsal nerve of the penis in males or the clitoris in females. This branch supplies sensory fibers to the glans penis or clitoris, contributing to the perception of touch and pleasure in these highly sensitive areas.
Superficial Perineal Nerve: The superficial perineal nerve is yet another branch of the perineal nerve. It provides sensory innervation to the perineal muscles, scrotum in males, and labia majora in females. This branch is responsible for transmitting sensations of touch, pressure, and temperature from these areas.
Functions of the Perineal Nerve
The perineal nerve serves both motor and sensory functions, playing a crucial role in maintaining pelvic floor health and overall well-being.
Motor Function: Motor fibers of the perineal nerve control the contraction of various muscles involved in maintaining continence. These muscles include the external anal sphincter, bulbospongiosus, and ischiocavernosus muscles. The coordinated contraction of these muscles ensures proper control over bowel and bladder movements, contributing to continence.
Sensory Function: Sensory fibers of the perineal nerve enable the perception of touch, temperature, and pressure in the perineal region. This allows individuals to have a sense of their surroundings and respond appropriately to various stimuli. Sensory information from the perineal nerve is crucial for sexual pleasure, as it contributes to the perception of touch and pleasure in the genital area.
In conclusion, the perineal nerve is a complex and important nerve that branches out to various structures in the perineal region. Its branches provide sensory innervation to specific areas and play a crucial role in maintaining continence and sexual function. Understanding the detailed anatomy and functions of the perineal nerve is essential for healthcare professionals and individuals seeking to maintain optimal pelvic floor health.
Disorders Related to the Perineal Nerve
Unfortunately, the perineal nerve is susceptible to various disorders that can disrupt its normal functioning. It is crucial to be aware of these disorders and their associated symptoms for early detection and prompt medical intervention.
The perineal nerve is a branch of the pudendal nerve, which originates from the sacral plexus. It provides sensory innervation to the perineum, a region located between the anus and the external genitalia. The perineum plays a vital role in various bodily functions, including urination, defecation, and sexual activity.
One common disorder related to the perineal nerve is perineal neuropathy. This condition occurs when the nerve is damaged or compressed, leading to a disruption in its normal signaling. Perineal neuropathy can be caused by various factors, including trauma, prolonged pressure on the nerve, infections, and certain medical conditions such as diabetes.
Common Symptoms of Perineal Nerve Damage
Perineal nerve damage can manifest in a variety of symptoms, such as numbness or tingling in the perineal region, urinary or fecal incontinence, loss of sensation during sexual activity, and muscle weakness in the pelvic floor. These symptoms can significantly impact an individual’s quality of life and may require comprehensive medical management.
Numbness or tingling in the perineal region can be distressing and may affect daily activities such as sitting or walking. Urinary or fecal incontinence, on the other hand, can lead to embarrassment and social isolation. Loss of sensation during sexual activity can impact both physical pleasure and emotional well-being. Muscle weakness in the pelvic floor can result in difficulties with bladder and bowel control.
It is essential to recognize these symptoms and promptly consult with a healthcare professional for accurate diagnosis and appropriate management strategies. Early intervention can help prevent further nerve damage and improve the chances of recovery.
Diagnostic Techniques for Perineal Nerve Disorders
When perineal nerve disorders are suspected, healthcare providers employ various diagnostic techniques to confirm the condition. These may include medical history assessments, physical examinations, nerve conduction studies, and imaging tests.
During a medical history assessment, the healthcare professional will inquire about the patient’s symptoms, medical history, and any potential risk factors. This information helps in narrowing down the possible causes of the perineal nerve disorder.
Physical examinations play a crucial role in evaluating the perineal region and assessing the function of the nerve. The healthcare provider may perform sensory tests, muscle strength assessments, and reflex tests to identify any abnormalities.
Nerve conduction studies are another diagnostic tool used to evaluate the electrical conduction of the perineal nerve. This test measures the speed and strength of nerve signals, helping to identify any disruptions or abnormalities in the nerve’s functioning.
In some cases, imaging tests such as magnetic resonance imaging (MRI) or ultrasound may be recommended. These tests can provide detailed images of the perineal region, helping to identify any structural abnormalities or sources of nerve compression.
It is important to undergo these diagnostic procedures under the guidance of a qualified healthcare professional. They will interpret the results and develop an appropriate treatment plan tailored to the individual’s specific condition and needs.
Treatment Options for Perineal Nerve Disorders
Perineal nerve disorders can cause significant discomfort and impact a person’s quality of life. Fortunately, there are several treatment approaches available to address these conditions. The choice of treatment depends on various factors, including the underlying cause, severity of symptoms, and individual patient factors.
Non-Surgical Treatments
Non-surgical treatments for perineal nerve disorders focus on alleviating symptoms, improving nerve function, and enhancing overall quality of life. Physical therapy is often recommended as a first-line treatment. This may involve exercises and stretches targeted at strengthening the muscles surrounding the perineal area and improving nerve function.
In addition to physical therapy, medication management is another non-surgical treatment option. Medications such as pain relievers, anti-inflammatory drugs, and nerve pain medications may be prescribed to help manage symptoms and reduce discomfort.
Lifestyle modifications can also play a significant role in managing perineal nerve disorders. These may include avoiding activities that exacerbate symptoms, maintaining a healthy weight, practicing good posture, and using ergonomic equipment to reduce pressure on the perineal area.
Furthermore, nerve stimulation techniques can be employed as part of the treatment plan. These techniques aim to stimulate the affected nerves and promote nerve regeneration. Electrical nerve stimulation, transcutaneous electrical nerve stimulation (TENS), and acupuncture are some examples of nerve stimulation techniques that may be used.
It is important to note that the effectiveness of non-surgical treatments may vary depending on the individual and the specific condition. Consulting with a healthcare professional is crucial to determine the most suitable treatment plan tailored to the patient’s needs.
Surgical Interventions
In some cases, non-surgical treatments may not provide adequate relief, and surgical interventions may be necessary to address the underlying cause of perineal nerve disorders. Surgical procedures can range from nerve decompression or repair to other specialized interventions tailored to the individual’s specific needs.
Nerve decompression surgery involves relieving pressure on the affected nerves, which can help alleviate symptoms and restore normal nerve function. This procedure may be performed using minimally invasive techniques, such as laparoscopy, or through open surgery, depending on the severity of the condition.
In cases where nerve damage is present, nerve repair surgery may be considered. This involves reconnecting or grafting damaged nerves to restore their function. The success of nerve repair surgery depends on various factors, including the extent of nerve damage and the patient’s overall health.
Other specialized surgical interventions may be recommended based on the specific underlying cause of the perineal nerve disorder. These procedures aim to address the root cause of the condition and provide long-term relief.
It is important for individuals considering surgical interventions to have a detailed discussion with a healthcare professional. This will help them understand the potential risks, benefits, and expected outcomes of the procedures, allowing them to make an informed decision regarding their treatment.
Prevention and Management of Perineal Nerve Disorders
While some perineal nerve disorders may be unavoidable, adopting preventive measures and management strategies can optimize overall nerve health and reduce the risk of complications.
Perineal nerve disorders can be caused by various factors, including trauma, compression, or inflammation of the nerve. By understanding the underlying causes and implementing appropriate preventive measures, individuals can take proactive steps towards maintaining optimal nerve health.
Lifestyle Changes for Better Nerve Health
Maintaining a healthy lifestyle can positively impact nerve health. Strategies may include regular exercise, a balanced diet, stress reduction techniques, and avoiding harmful substances. Regular exercise, such as walking, swimming, or yoga, can improve blood circulation and promote nerve health. A balanced diet rich in essential nutrients, vitamins, and minerals can provide the necessary building blocks for nerve tissue repair and regeneration.
In addition, stress reduction techniques, such as meditation, deep breathing exercises, or engaging in hobbies, can help lower stress levels, which can contribute to nerve damage. It is essential to consult with a healthcare professional before implementing any significant changes to your lifestyle, as they can provide personalized guidance based on individual needs and medical history.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation programs tailored to perineal nerve disorders can be instrumental in improving symptoms and restoring normal function. These programs often include exercises targeting the pelvic floor muscles and specialized techniques aimed at enhancing nerve conduction.
A qualified physical therapist can guide individuals through these programs and monitor their progress. They may use various techniques, such as manual therapy, electrical stimulation, or biofeedback, to stimulate nerve regeneration and improve muscle strength and coordination. Physical therapy sessions may also include education on proper body mechanics and ergonomics to prevent further nerve damage.
In addition to in-person physical therapy sessions, individuals may also benefit from home exercise programs prescribed by their physical therapist. These programs can help individuals maintain their progress and continue their rehabilitation journey outside of the clinic.
Alternative Therapies
In some cases, individuals with perineal nerve disorders may explore alternative therapies to complement traditional treatment approaches. These therapies can include acupuncture, chiropractic care, or herbal medicine.
Acupuncture, a traditional Chinese medicine practice, involves the insertion of thin needles into specific points of the body to stimulate nerve function and promote healing. Chiropractic care focuses on the alignment of the spine and musculoskeletal system, which can indirectly affect nerve health. Herbal medicine utilizes plant-based remedies to address various health conditions, including nerve disorders.
It is important to consult with healthcare professionals experienced in these alternative therapies to ensure their safety and effectiveness, as well as to avoid potential interactions with other medications or treatments.
By adopting preventive measures, engaging in physical therapy and rehabilitation, and exploring alternative therapies under professional guidance, individuals with perineal nerve disorders can take an active role in managing their condition and optimizing their nerve health.
Future Research Directions in Perineal Nerve Health
As the field of medical research continues to advance, ongoing investigations into perineal nerve health are expected to unlock new insights and treatment modalities.
Emerging Treatments and Therapies
Researchers are exploring promising avenues for the treatment of perineal nerve disorders. This includes potential pharmacological interventions, regenerative medicine approaches, and novel therapies targeting nerve regeneration and pain management. Stay informed about advancements in the field by consulting reputable medical sources and discussing emerging treatment options with healthcare professionals.
The Role of Technology in Perineal Nerve Health
Technological advancements have the potential to revolutionize the diagnosis and treatment of perineal nerve disorders. Innovations such as neurostimulation devices, virtual reality-assisted rehabilitation, and advanced imaging techniques may enhance our capabilities in managing these conditions. However, the application of technology in healthcare requires careful consideration and guidance from healthcare professionals.
In conclusion, understanding perineal nerve anatomy is crucial for comprehending its role in maintaining essential bodily functions. By familiarizing ourselves with the perineal nerve’s structure, functions, related disorders, treatment options, and strategies for prevention and management, we can strive for optimal nerve health. Furthermore, staying informed about future research directions offers hope for advancements in diagnosis, treatment, and overall improvement in perineal nerve health. Remember, always consult with a knowledgeable healthcare professional to address individual concerns and receive appropriate medical guidance.