Perineal nerve pain is a condition that can greatly impact one’s quality of life. The perineal nerve is a branch of the pudendal nerve, which originates in the sacral plexus. It innervates the perineum, a region located between the anus and genitals, and is responsible for providing sensation to this area. In this article, we will explore the various aspects of perineal nerve pain, including its causes, symptoms, diagnostic procedures, treatment options, and tips for living with this condition.
What is Perineal Nerve Pain?
Perineal nerve pain, also known as perineal neuralgia, is a type of chronic pain that originates from the perineal nerve or its surrounding structures. This pain can range from mild discomfort to severe and debilitating, affecting daily activities such as sitting, walking, and sexual intercourse.
Perineal nerve pain is a complex condition that can have a significant impact on a person’s quality of life. It can be challenging to diagnose and treat, as the underlying causes and mechanisms are not always clear-cut. However, understanding the anatomy of the perineal nerve and the common conditions associated with perineal nerve pain can provide valuable insights.
Anatomy of the Perineal Nerve
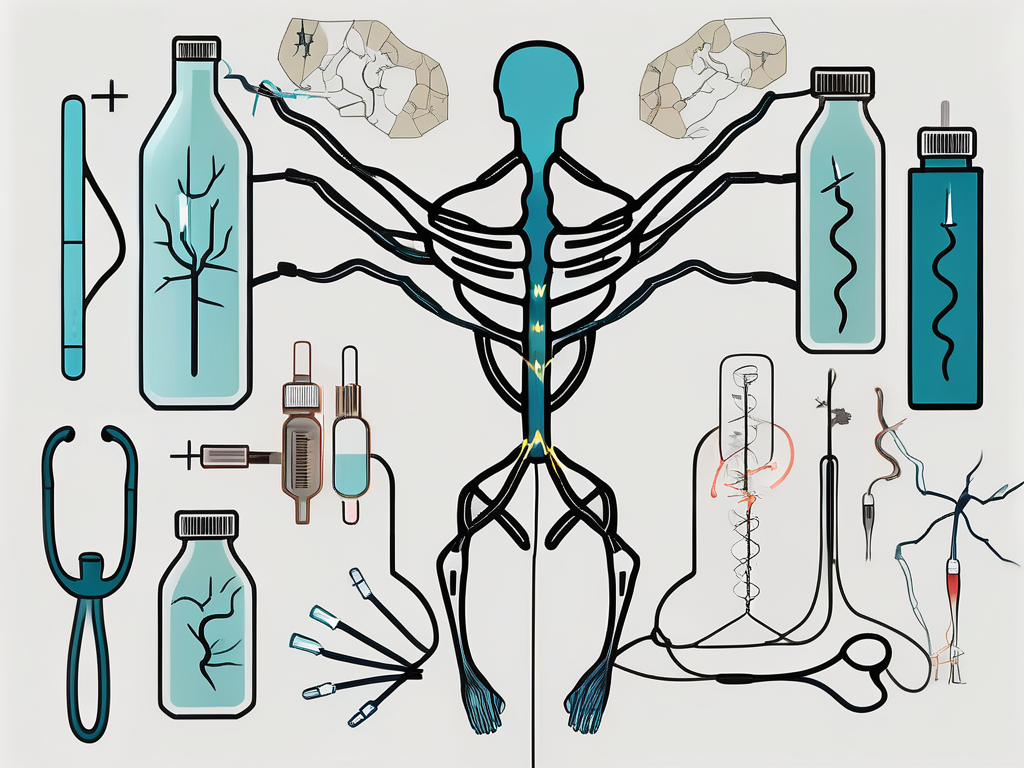
To understand perineal nerve pain, it is important to have a basic understanding of the anatomy of the perineal nerve. The perineal nerve arises from the pudendal nerve, which is derived from the sacral plexus. It travels through the pelvis and supplies sensation to the perineum, including the anus and external genitalia.
The perineal nerve plays a crucial role in the normal functioning of the pelvic region. It carries sensory information from the perineum to the brain, allowing us to perceive touch, temperature, and pain in this area. It also innervates the muscles responsible for controlling bowel and bladder function.
Any disruption or damage to the perineal nerve can lead to altered sensation, pain, and dysfunction in the perineal region. This can manifest as perineal nerve pain, which can be localized or radiate to other areas of the body.
Common Conditions Related to Perineal Nerve Pain
Perineal nerve pain can occur as a result of various underlying conditions. Understanding these conditions can help healthcare professionals identify and manage perineal nerve pain effectively.
Pudendal Neuralgia: Pudendal neuralgia is a condition characterized by chronic pain in the perineal region, often caused by irritation or compression of the pudendal nerve. This can result from trauma, prolonged sitting, pelvic surgery, or childbirth.
Perineal Trauma or Injury: Trauma or injury to the perineum, such as during childbirth or accidents, can damage the perineal nerve and lead to persistent pain.
Pelvic Floor Dysfunction: Dysfunction of the pelvic floor muscles, which support the organs in the pelvis, can contribute to perineal nerve pain. Conditions such as pelvic floor muscle spasms or weakness can lead to nerve compression or irritation.
Pelvic Inflammatory Disease: Inflammation of the pelvic organs, often caused by infection, can result in perineal nerve pain. Conditions like sexually transmitted infections or chronic pelvic inflammatory disease can lead to persistent discomfort in the perineal region.
Endometriosis and Prostate Disorders: Certain medical conditions, such as endometriosis in women or prostate disorders in men, can cause perineal nerve pain. These conditions involve abnormal growth or inflammation of tissues in the pelvic region, which can irritate the perineal nerve.
It is important to note that perineal nerve pain can also be idiopathic, meaning that no specific cause can be identified. In such cases, a comprehensive evaluation and individualized treatment approach are necessary to manage the pain effectively.
Causes of Perineal Nerve Pain
Perineal nerve pain can be caused by a variety of factors. Understanding these causes can help individuals and healthcare professionals identify and manage the condition effectively.
Perineal nerve pain, also known as pudendal neuralgia, can be a debilitating condition that affects the perineum, the area between the genitals and the anus. It can cause chronic pain, discomfort, and even difficulty with daily activities. While the exact cause of perineal nerve pain may vary from person to person, there are several common factors that can contribute to its development.
Physical Trauma and Injury
Physical trauma or injury to the perineum, such as a fall or direct impact, can result in perineal nerve pain. This can lead to nerve compression or damage, triggering persistent pain and discomfort. In some cases, the trauma may be obvious, such as a sports injury or a fall from a bicycle. However, in other cases, the trauma may be less apparent, such as from childbirth or prolonged pressure on the perineum during certain activities.
It is important to note that perineal nerve pain can also be caused by surgical procedures, such as pelvic surgery or procedures involving the perineum. These procedures can sometimes result in nerve damage or irritation, leading to chronic pain.
Medical Conditions and Diseases
Various medical conditions and diseases can be associated with perineal nerve pain. These include but are not limited to pelvic inflammatory disease, coccydynia (tailbone pain), interstitial cystitis, and certain gynecological or urological disorders. These conditions can cause inflammation, nerve compression, or damage in the perineal area, leading to persistent pain and discomfort.
In addition, certain infections, such as sexually transmitted infections or urinary tract infections, can also contribute to perineal nerve pain. These infections can cause inflammation and irritation in the perineum, affecting the nerves and causing pain.
Lifestyle Factors and Perineal Nerve Pain
Lifestyle factors such as prolonged sitting, cycling, excessive exercise, or repetitive strain on the perineum can also contribute to perineal nerve pain. Postpartum women, athletes, and individuals with occupations that require extended periods of sitting or strenuous physical activity may be at an increased risk.
For example, cyclists may experience perineal nerve pain due to the constant pressure and friction on the perineum during long rides. Similarly, individuals who sit for prolonged periods, such as office workers or truck drivers, may develop perineal nerve pain due to the continuous pressure on the area.
It is important to note that lifestyle factors alone may not be the sole cause of perineal nerve pain, but they can contribute to its development or exacerbation. It is often a combination of factors, including lifestyle, medical conditions, and trauma, that contribute to the onset and persistence of perineal nerve pain.
In conclusion, perineal nerve pain can have various causes, including physical trauma, medical conditions, and lifestyle factors. Identifying and understanding these causes can help individuals and healthcare professionals develop effective strategies for managing and treating perineal nerve pain.
Recognizing the Symptoms of Perineal Nerve Pain
Identifying the symptoms of perineal nerve pain is crucial for early diagnosis and management. The symptoms can vary from person to person and may include:
Physical Symptoms
Physical symptoms of perineal nerve pain may include chronic pelvic or perineal pain, numbness or tingling sensation in the perineal area, and pain worsening with prolonged sitting or certain activities.
Chronic pelvic or perineal pain can be described as a persistent discomfort or ache in the lower abdominal or genital region. This pain can range from mild to severe and may be constant or intermittent. It can greatly impact a person’s daily activities and quality of life.
In addition to pain, individuals with perineal nerve pain may experience numbness or a tingling sensation in the perineal area. This can manifest as a loss of sensation or a “pins and needles” feeling. It can be localized or radiate to the surrounding areas.
Furthermore, perineal nerve pain may worsen with prolonged sitting or certain activities. Sitting for extended periods can put pressure on the perineal area, exacerbating the pain. Activities that involve repetitive or strenuous movements of the pelvic region, such as cycling or weightlifting, can also trigger or intensify the pain.
Emotional and Psychological Symptoms
Perineal nerve pain can also have emotional and psychological effects. Many individuals with this condition may experience anxiety, depression, frustration, and a reduced quality of life due to persistent pain and limited functioning.
The constant presence of pain can lead to feelings of anxiety and distress. Individuals may worry about the impact of the pain on their daily lives, relationships, and overall well-being. The uncertainty of when the pain will subside or if it will worsen can contribute to heightened levels of anxiety.
Depression can also be a common emotional symptom experienced by individuals with perineal nerve pain. The chronic pain can lead to feelings of sadness, hopelessness, and a loss of interest in previously enjoyed activities. The combination of physical discomfort and emotional distress can create a cycle of negative emotions that further impact a person’s mental well-being.
Frustration is another emotional symptom that individuals with perineal nerve pain may experience. The persistent nature of the pain, along with limited treatment options, can lead to feelings of helplessness and frustration. This frustration may stem from the challenges of managing daily activities while dealing with the pain.
Ultimately, the emotional and psychological symptoms associated with perineal nerve pain can significantly affect a person’s quality of life. The pain and its impact on physical and emotional well-being can lead to social isolation, reduced productivity, and a decreased overall sense of happiness and fulfillment.
Diagnostic Procedures for Perineal Nerve Pain
Diagnosing perineal nerve pain often involves a comprehensive evaluation, including medical history, physical examination, and specific diagnostic tests.
Medical History and Physical Examination
A detailed medical history helps healthcare professionals understand the context and potential causes of perineal nerve pain. This includes gathering information about the patient’s symptoms, their duration, and any factors that may aggravate or alleviate the pain. Additionally, a physical examination may be performed to assess the pelvic region, including the perineum, to identify any abnormalities or areas of tenderness. The healthcare professional may palpate the perineal area to check for any signs of inflammation, swelling, or muscle tension. They may also evaluate the patient’s posture and gait to identify any potential contributing factors to the nerve pain.
During the physical examination, the healthcare professional may also assess the patient’s sensation and reflexes in the perineal area. This can help determine if there is any sensory loss or abnormal reflexes, which may indicate nerve damage or compression. The examination may also involve assessing the strength and coordination of the pelvic floor muscles, as weakness or dysfunction in these muscles can contribute to perineal nerve pain.
Imaging Tests
Imaging tests, such as magnetic resonance imaging (MRI), computed tomography (CT) scan, or ultrasound, may be recommended to visualize the pelvic structures and identify any structural abnormalities or nerve compression. These imaging techniques can provide detailed images of the bones, muscles, and nerves in the pelvic region, allowing healthcare professionals to identify any potential sources of perineal nerve pain. MRI and CT scans are particularly useful in detecting structural abnormalities, such as herniated discs, tumors, or cysts, that may be compressing the perineal nerve. Ultrasound, on the other hand, can provide real-time images and help assess the blood flow to the perineal area, which can be useful in diagnosing conditions like pudendal artery entrapment.
Nerve Conduction Studies
Nerve conduction studies are specialized tests that evaluate the function and integrity of the nerves. These tests may be conducted to assess the conduction of the perineal nerve and identify any abnormalities or damage. During a nerve conduction study, small electrodes are placed on the skin overlying the perineal nerve, and a mild electrical stimulus is applied. The response of the nerve is then measured, allowing healthcare professionals to assess the speed and strength of the nerve conduction. Abnormal results, such as a slowed conduction velocity or reduced amplitude, may indicate nerve damage or compression. Nerve conduction studies can help differentiate between nerve entrapment, nerve injury, or other underlying conditions contributing to perineal nerve pain.
In addition to these diagnostic procedures, healthcare professionals may also consider other tests or consultations based on the individual patient’s symptoms and medical history. These may include blood tests to rule out underlying systemic conditions, consultation with a pelvic floor physical therapist for further evaluation of muscle dysfunction, or referral to a specialist for further evaluation and treatment.
Treatment Options for Perineal Nerve Pain
The management of perineal nerve pain usually involves a multimodal approach to target different aspects of the condition and improve quality of life.
Perineal nerve pain, also known as pudendal neuralgia, can be a debilitating condition that affects the perineum, which is the area between the anus and genitals. It can cause chronic pain, discomfort, and difficulty with daily activities.
When it comes to treating perineal nerve pain, healthcare professionals have several options to consider. These options range from medication therapies to physical therapy and rehabilitation, and in severe cases, surgical interventions.
Medication Therapies
Medication therapies may be prescribed by healthcare professionals to help manage the pain associated with perineal nerve pain. These may include nonsteroidal anti-inflammatory drugs (NSAIDs), nerve pain medications, muscle relaxants, or, in some cases, tricyclic antidepressants.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and provide temporary relief from pain. Nerve pain medications, such as gabapentin or pregabalin, work by targeting the nerves and reducing their sensitivity to pain signals. Muscle relaxants can help alleviate muscle spasms and tension in the pelvic region, which can contribute to perineal nerve pain. Tricyclic antidepressants, despite their name, can also be effective in managing nerve pain by blocking pain signals in the brain.
It is important to note that medication therapies may vary depending on the individual’s specific symptoms and medical history. Healthcare professionals will carefully assess each case to determine the most suitable medication regimen.
Physical Therapy and Rehabilitation
Physical therapy can play a significant role in the management of perineal nerve pain. Pelvic floor physical therapy, in particular, aims to improve muscle strength, flexibility, and coordination within the pelvic region, reducing pain and improving overall function.
During pelvic floor physical therapy, a trained therapist will guide the individual through exercises that target the muscles in the pelvic floor. These exercises may include kegel exercises, stretches, and relaxation techniques. The therapist may also provide education on proper body mechanics and postural adjustments to minimize pain and discomfort.
In addition to pelvic floor physical therapy, other forms of physical therapy, such as nerve mobilization techniques and myofascial release, may be incorporated to address any underlying nerve entrapment or muscle imbalances that contribute to perineal nerve pain.
It is important to note that physical therapy for perineal nerve pain is typically a long-term commitment. Regular sessions and consistent adherence to prescribed exercises are essential for optimal results.
Surgical Interventions
In severe cases where conservative treatments have not provided sufficient relief, surgical interventions may be considered. Nerve decompression surgery or other procedures may be performed to relieve nerve entrapment or remove sources of compression.
Nerve decompression surgery involves identifying and releasing any areas of nerve entrapment or compression in the pelvic region. This can help alleviate pressure on the perineal nerve and reduce pain. Other surgical procedures, such as neurectomy or nerve blocks, may also be considered depending on the individual’s specific condition.
It is important to note that surgical interventions for perineal nerve pain are typically reserved for cases where other treatment options have been exhausted. The decision to undergo surgery should be carefully considered, and individuals should consult with their healthcare professionals to weigh the potential risks and benefits.
In conclusion, the management of perineal nerve pain involves a comprehensive approach that addresses the underlying causes and symptoms. Medication therapies, physical therapy, and surgical interventions are all potential treatment options that healthcare professionals may consider based on the individual’s specific condition. With proper diagnosis and a tailored treatment plan, individuals with perineal nerve pain can find relief and improve their quality of life.
Living with Perineal Nerve Pain
Coping with perineal nerve pain can be challenging, both physically and emotionally. However, there are strategies and resources available to help individuals manage their condition and improve their quality of life.
Coping Strategies and Pain Management
Implementing effective coping strategies can greatly enhance one’s ability to manage perineal nerve pain. Techniques such as mindfulness, relaxation exercises, and stress management techniques can help reduce physical and emotional symptoms associated with chronic pain. Additionally, adapting daily activities, using ergonomic support, and maintaining a healthy lifestyle can positively impact overall well-being.
Support and Resources for Patients
Seeking support from healthcare professionals, support groups, and online communities can be invaluable for individuals living with perineal nerve pain. These resources can provide education, emotional support, and practical tips for managing the condition. It is always recommended to consult with a healthcare professional to determine the most appropriate course of action based on individual needs and circumstances.
Conclusion
Understanding the causes, symptoms, and treatment options for perineal nerve pain is crucial for individuals experiencing this condition. By recognizing the signs and seeking appropriate medical guidance, individuals can take proactive steps towards managing their pain and improving their overall well-being. Remember, perineal nerve pain is a complex condition, and it is essential to consult with a healthcare professional for personalized advice and treatment.