The perineal nerve plays a crucial role in the functioning of the human body. Its intricate anatomy and physiology contribute to various bodily processes, making it essential to have an understanding of its functions and potential disorders. In this comprehensive guide, we will delve into the details of the perineal nerve, explore its connection with the pudendal nerve, discuss disorders affecting it, examine diagnostic procedures, explore treatment options, and look into the future of perineal nerve research.
Defining the Perineal Nerve: Anatomy and Physiology
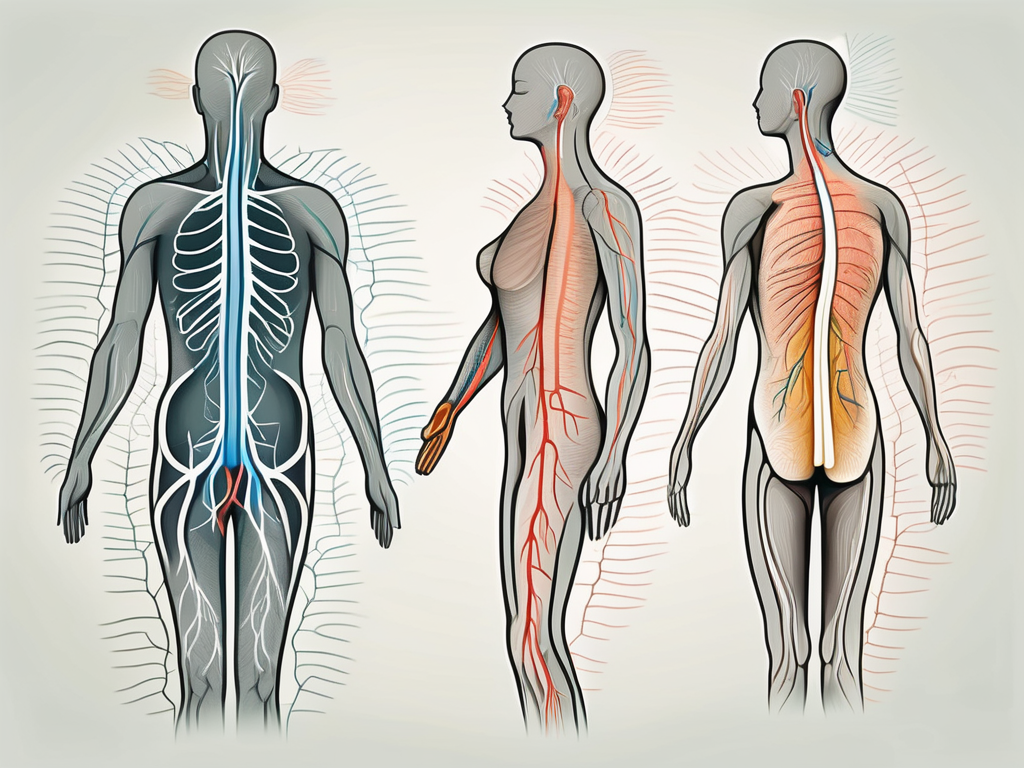
The perineal nerve is a branch of the pudendal nerve, which originates from the sacral plexus. It supplies innervation to the perineum, a diamond-shaped region between the pubic symphysis, coccyx, ischial tuberosities, and the posterior margin of the anus. In males, the perineum includes the scrotum, while in females, it encompasses the vulva.
The perineal nerve controls sensory and motor functions in this region. Sensory information from the perineum is transmitted by sensory fibers, while motor fibers enable the contraction of various muscles within the perineal area.
The perineal nerve is a fascinating component of the human body’s nervous system. Let’s delve deeper into its role and significance.
The Role of the Perineal Nerve in the Human Body
The perineal nerve plays a vital role in sexual function, as it supplies sensory information to the genitals. It is responsible for transmitting sensations of touch, pressure, temperature, and pain from the genital area to the brain. This intricate network of nerves ensures that our experiences of pleasure, discomfort, and pain in the perineal region are properly communicated and interpreted by the brain.
Moreover, the perineal nerve also controls the contraction of the perineal muscles, allowing for the coordination of movements during urination, defecation, and sexual activity. Without the perineal nerve, these essential bodily functions would be compromised, leading to significant difficulties in everyday life.
Understanding the role of the perineal nerve highlights its importance in maintaining overall well-being and quality of life.
The Connection Between the Perineal Nerve and the Pudendal Nerve
The perineal nerve and the pudendal nerve are closely related and often discussed interchangeably. While the pudendal nerve branches off into several nerves, including the perineal nerve, its overall function is to innervate the perineum. The perineal nerve, along with other branches of the pudendal nerve, works collectively to ensure proper functioning of the perineum.
It is interesting to note that the pudendal nerve, from which the perineal nerve originates, also supplies innervation to other important structures in the pelvic region, such as the external anal sphincter and the muscles of the pelvic floor. This interconnected network of nerves showcases the complexity and intricacy of the human body’s nervous system.
By understanding the connection between the perineal nerve and the pudendal nerve, we gain a deeper appreciation for the coordination and cooperation required among various nerves to ensure the proper functioning of our bodies.
Disorders and Conditions Affecting the Perineal Nerve
Perineal nerve dysfunction can lead to a range of disorders and conditions that can significantly impact an individual’s quality of life. Understanding the symptoms and common conditions associated with perineal nerve dysfunction is crucial in identifying and seeking appropriate medical attention.
The perineal nerve, also known as the pudendal nerve, is a crucial nerve that provides sensory and motor functions to the perineal region. This region includes the area between the genitals and the anus, and any dysfunction in this nerve can have profound effects on a person’s daily life.
Symptoms of Perineal Nerve Dysfunction
Perineal nerve dysfunction may manifest through various symptoms, including pain, numbness, tingling, or a burning sensation in the perineal region. These symptoms can range from mild discomfort to severe pain, making it challenging for individuals to perform routine activities.
In addition to sensory symptoms, perineal nerve dysfunction can also affect motor functions. Patients may experience difficulty in controlling bowel or bladder movements, leading to incontinence or urinary retention. Sexual dysfunction is another common symptom, as the perineal nerve plays a crucial role in sexual arousal and orgasm.
It’s important to note that these symptoms may also indicate other underlying conditions, necessitating a comprehensive evaluation by a healthcare professional to determine the underlying cause. A thorough medical history, physical examination, and diagnostic tests may be necessary to accurately diagnose perineal nerve dysfunction.
Common Conditions: From Perineal Nerve Entrapment to Neuropathy
A variety of conditions can affect the perineal nerve, each with its own set of causes and symptoms. Perineal nerve entrapment occurs when the nerve gets compressed or trapped, leading to symptoms such as pain and sensory changes.
Perineal nerve compression can result from various factors, including trauma, repetitive motions, or prolonged pressure on the nerve. Activities such as cycling, horseback riding, or sitting for extended periods can increase the risk of nerve compression. It may cause symptoms similar to entrapment, such as pain, numbness, or tingling in the perineal region.
Perineal neuropathy refers to damage or dysfunction of the perineal nerve, resulting from various causes such as diabetes, infections, or trauma. Diabetes, in particular, can lead to nerve damage over time, affecting both sensory and motor functions in the perineal region.
Other conditions that can affect the perineal nerve include pelvic floor dysfunction, pelvic inflammatory disease, and certain types of cancer. These conditions can cause inflammation or damage to the nerve, leading to a wide range of symptoms.
Whether experiencing symptoms related to perineal nerve entrapment, compression, or neuropathy, seeking professional medical advice is imperative for an accurate diagnosis and appropriate treatment. Treatment options may include physical therapy, medications, nerve blocks, or, in severe cases, surgical intervention.
Living with perineal nerve dysfunction can be challenging, but with proper medical management and support, individuals can find relief from their symptoms and improve their quality of life. It’s essential to consult with a healthcare professional to develop a personalized treatment plan that addresses the underlying cause and provides effective symptom management.
Diagnostic Procedures for Perineal Nerve Dysfunction
Diagnosing perineal nerve dysfunction requires a comprehensive evaluation, including a thorough physical examination, patient history, and sometimes, advanced diagnostic tools.
Perineal nerve dysfunction can cause a range of symptoms, including pain, numbness, or tingling in the perineal region. These symptoms can significantly impact a person’s quality of life and may be indicative of an underlying issue that needs to be addressed.
Physical Examination and Patient History
During a physical examination, a healthcare professional will assess the perineal region, looking for any signs of inflammation, tenderness, or other abnormalities. They will gently palpate the area, checking for any areas of increased sensitivity or discomfort.
In addition to the physical examination, the healthcare professional will also conduct a detailed patient history. This involves asking the patient questions about their symptoms, when they started, and any factors that may exacerbate or alleviate the symptoms.
Patient history is equally important in diagnosing perineal nerve dysfunction, as it helps identify potential underlying causes. Patients may be asked about their medical history, previous traumas, existing medical conditions, or any repetitive activities that may have contributed to their symptoms.
For example, a patient who frequently engages in activities that put pressure on the perineal region, such as cycling or horseback riding, may be at a higher risk of developing perineal nerve dysfunction.
Advanced Diagnostic Tools: Imaging and Electromyography
In complex cases or when further investigation is necessary, advanced diagnostic tools may be employed. Imaging techniques such as magnetic resonance imaging (MRI) or ultrasound can help visualize the perineal nerve and surrounding structures, aiding in the assessment and identification of potential abnormalities or compressions.
An MRI scan can provide detailed images of the perineal region, allowing healthcare professionals to assess the nerve’s integrity and identify any potential sources of nerve compression, such as tumors or herniated discs.
Electromyography (EMG) is another useful diagnostic tool that evaluates the electrical activity of muscles associated with the perineal nerve. During an EMG, small electrodes are inserted into the muscles surrounding the perineal region, and the electrical signals produced by these muscles are recorded and analyzed.
EMG can help determine the functionality of the nerve and assess any potential damage or dysfunction. It can also help differentiate between perineal nerve dysfunction and other conditions that may present with similar symptoms.
It is important to note that these diagnostic procedures should be conducted under the supervision of qualified healthcare professionals who specialize in neurological or pelvic floor disorders. They have the expertise and knowledge to interpret the results accurately and develop an appropriate treatment plan based on the findings.
Treatment Options for Perineal Nerve Disorders
When it comes to treating perineal nerve disorders, a multidisciplinary approach involving multiple healthcare professionals may be necessary. Treatment options range from non-surgical interventions to surgical procedures, depending on the severity and underlying cause of the condition.
Perineal nerve disorders can significantly impact a person’s quality of life, causing pain, discomfort, and limitations in daily activities. Therefore, finding the most suitable treatment approach is crucial to alleviate symptoms and improve overall well-being.
Non-Surgical Treatments: Medication and Physical Therapy
In less severe cases, non-surgical treatment options may be recommended. Medications, such as pain relievers or nerve-specific medications, can help manage pain and alleviate symptoms associated with perineal nerve dysfunction.
Physical therapy may also play a vital role in the treatment of perineal nerve disorders. Skilled physical therapists can develop personalized exercise programs targeting the affected muscles and nerves. These exercises aim to improve muscle strength, coordination, and overall function within the perineal region.
In addition to exercises, physical therapists may employ various techniques such as manual therapy, electrical stimulation, and biofeedback to enhance treatment outcomes. These non-invasive interventions can help restore normal nerve function and alleviate symptoms.
It is crucial to consult with a healthcare professional before starting any medication or physical therapy regimen to ensure proper guidance and supervision tailored to individual needs. They can assess the severity of the condition and recommend the most appropriate treatment plan.
Surgical Interventions for Perineal Nerve Disorders
In more severe or refractory cases, surgical interventions may be considered. Surgical options for perineal nerve disorders can involve decompression of the nerve, removal of scar tissue or tumors compressing the nerve, nerve grafting, or nerve stimulation techniques.
Decompression surgery aims to relieve pressure on the perineal nerve by removing any structures or tissues that may be compressing it. This can help restore normal nerve function and alleviate symptoms. In cases where scar tissue or tumors are causing nerve compression, surgical removal may be necessary to provide relief.
Nerve grafting is another surgical technique that involves replacing damaged or injured sections of the perineal nerve with healthy nerve tissue. This procedure can help restore nerve function and improve symptoms in certain cases.
Nerve stimulation techniques, such as neuromodulation, can also be employed in the treatment of perineal nerve disorders. These techniques involve the use of electrical impulses to stimulate the affected nerves, helping to alleviate pain and improve function.
It is essential to recognize that each surgical intervention carries its own risks and benefits, and proper evaluation by trained healthcare professionals is required to determine the most appropriate course of action. The decision to undergo surgery should be made in close consultation with a specialist who can provide detailed information and guidance based on the individual’s specific condition.
In conclusion, the treatment options for perineal nerve disorders vary depending on the severity and underlying cause of the condition. Non-surgical interventions, such as medication and physical therapy, can be effective in managing symptoms and improving function. However, in more severe cases, surgical interventions may be necessary to alleviate nerve compression and restore normal nerve function. Consulting with a healthcare professional is crucial to determine the most suitable treatment approach for each individual.
The Future of Perineal Nerve Research
Perineal nerve research continues to evolve, promising potential advancements and emerging therapies that may revolutionize the understanding and treatment of perineal nerve disorders.
Emerging Therapies and Techniques
Ongoing research explores various emerging therapies for perineal nerve disorders. These include regenerative medicine techniques that aim to repair damaged nerves, such as stem cell therapy or growth factor therapy. Stem cell therapy, for example, involves the use of specialized cells that have the potential to regenerate and repair damaged tissues. This therapy holds great promise for perineal nerve disorders, as it may help restore normal nerve function and alleviate symptoms.
In addition to regenerative medicine, other innovative approaches are also being investigated. Neuromodulation techniques, for instance, involve the use of electrical or chemical stimuli to modulate the activity of nerves. This can help regulate abnormal nerve signals and provide relief from symptoms. Gene therapy, on the other hand, aims to introduce specific genes into the body to correct genetic abnormalities that may be causing perineal nerve disorders. These emerging therapies offer exciting possibilities for the future of perineal nerve treatment.
The Impact of Technological Advancements on Perineal Nerve Treatment
Technological advancements are playing a crucial role in transforming the landscape of perineal nerve treatment. Advanced imaging techniques, such as magnetic resonance imaging (MRI) and ultrasound, provide healthcare professionals with detailed and accurate visualization of the perineal nerves. This enables precise diagnosis and targeted interventions, leading to improved patient outcomes.
Minimally invasive surgical procedures are also revolutionizing perineal nerve treatment. These procedures involve smaller incisions and specialized instruments, resulting in reduced pain, faster recovery, and fewer complications. For example, laparoscopic techniques allow surgeons to access the perineal nerves through small incisions, minimizing tissue damage and promoting quicker healing.
Furthermore, the integration of robotics and artificial intelligence in surgical procedures holds great promise for perineal nerve treatment. Robotic-assisted surgery allows for enhanced precision and control, enabling surgeons to perform intricate procedures with greater accuracy. Artificial intelligence algorithms can also assist in analyzing complex data and providing real-time feedback during surgery, further improving surgical outcomes.
However, it is important to note that these emerging therapies and advancements are still in the research and development phase. Extensive clinical trials and regulatory approvals are necessary before they can be widely implemented in clinical practice. Patients should consult with healthcare professionals who are up to date with the latest research and clinical practice guidelines to determine the most appropriate treatment plan for their specific condition.
In conclusion, understanding perineal nerve function is essential in comprehending the complex interplay between this nerve and the human body. From its anatomical and physiological aspects to the disorders that can affect it, a thorough understanding of the perineal nerve allows for accurate diagnosis and appropriate treatment. With ongoing research and advancements, the future of perineal nerve treatment holds the promise of improved outcomes and a better quality of life for those affected by perineal nerve disorders.