The deep perineal nerve is a crucial component of the human nervous system, playing a vital role in various physiological functions and clinical scenarios. Understanding its anatomy, physiological role, clinical significance, and treatment options is essential to comprehending the complexities associated with deep perineal nerve disorders. This comprehensive guide aims to shed light on these aspects and provide a platform for further discussions and research in this field.
Anatomy of the Deep Perineal Nerve
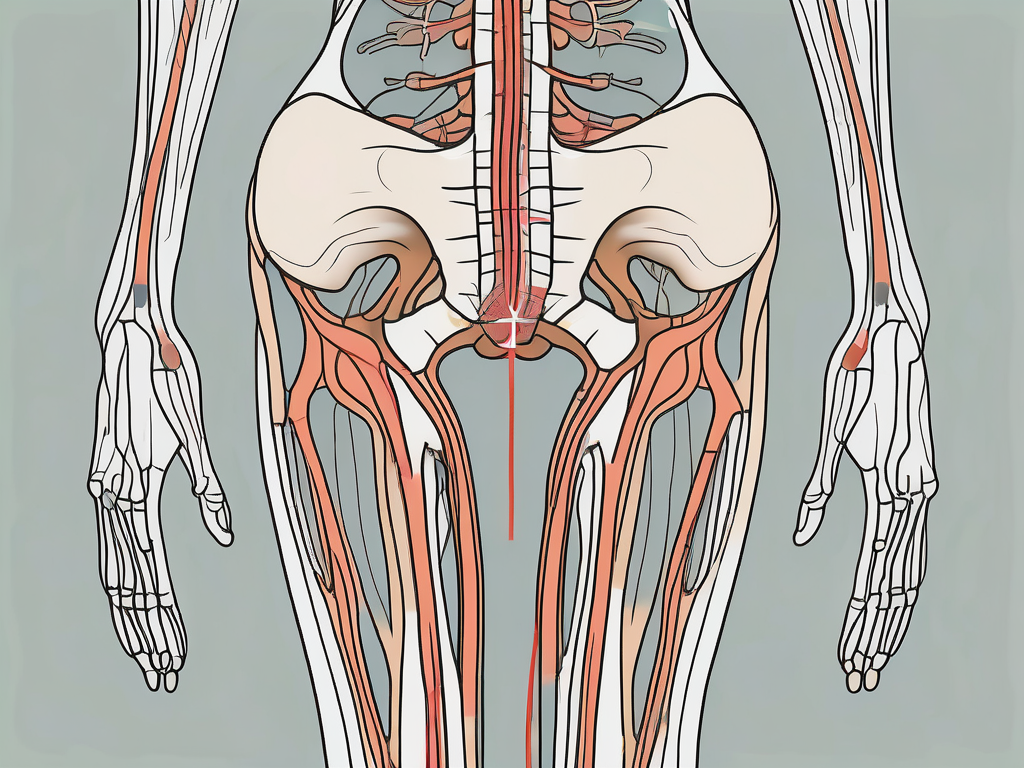
The deep perineal nerve, also known as the posterior branch of the pudendal nerve, arises from the sacral plexus, specifically from the S2 and S3 spinal nerve roots. It descends through the pelvis and innervates several structures involved in pelvic floor function, including the external urethral sphincter, urethral mucosa, and bulbospongiosus muscle.
The deep perineal nerve follows a complex pathway, traversing through the urogenital diaphragm and providing innervation to various structures within the male and female perineum. The nerve’s proximity to crucial anatomical elements such as the prostate gland and urethra underscores its significance in maintaining continence and sexual function.
The deep perineal nerve is a vital component of the perineal region, playing a crucial role in both motor and sensory functions. Let’s delve deeper into its origin, pathway, branches, and connections to gain a comprehensive understanding of its significance.
Origin and Pathway
The deep perineal nerve originates from the ventral rami of the sacral spinal nerves and emerges from the greater sciatic foramen. It then enters the pelvis through the lesser sciatic foramen, eventually joining the pudendal nerve. This intricate pathway allows the nerve to reach its target structures within the perineum.
As the deep perineal nerve courses through the pelvis, it sends out branches to innervate various muscles and tissues. One of its primary destinations is the external urethral sphincter, a crucial muscle responsible for voluntary control of urination. By providing innervation to this muscle, the deep perineal nerve enables individuals to maintain continence and regulate the flow of urine.
Furthermore, the deep perineal nerve also supplies sensory innervation to the urethral mucosa, ensuring proper sensation and feedback during urination. This sensory input plays a vital role in the coordination of bladder function and the perception of urinary urgency.
Branches and Connections
Throughout its course, the deep perineal nerve gives rise to various branches and forms important connections with adjacent nerves and structures. These connections contribute to the overall functionality and coordination of the perineal region.
One notable connection is with the dorsal nerve of the penis or clitoris, depending on the individual’s sex. This communication between the deep perineal nerve and the dorsal nerve contributes to the sensory innervation of the genitalia. It allows for the perception of touch, temperature, and other sensory modalities, enhancing sexual pleasure and overall genital sensation.
In addition to its connection with the dorsal nerve, the deep perineal nerve also interacts with the perineal branches of the posterior femoral cutaneous nerve. This interaction facilitates coordinated sensory feedback from the perineum and lower limb, ensuring proper sensation and proprioception in this region.
Overall, the deep perineal nerve’s branches and connections play a critical role in maintaining the functionality and integrity of the perineal region. Its intricate pathway and interactions with adjacent structures highlight its significance in both motor and sensory functions.
Physiological Role of the Deep Perineal Nerve
The deep perineal nerve serves both sensory and motor functions, playing a vital role in the normal functioning of the pelvic floor and associated structures.
The deep perineal nerve, also known as the pudendal nerve, is a crucial component of the peripheral nervous system. It originates from the sacral plexus, specifically from the S2, S3, and S4 nerve roots. This nerve provides innervation to various structures in the perineum, including the urethra, perineum, and external genitals.
Sensory Functions
The sensory branches of the deep perineal nerve transmit information from the urethra, perineum, and external genitals to the central nervous system. This feedback enables crucial processes such as the perception of touch, pain, and temperature.
When the deep perineal nerve is functioning optimally, individuals can accurately perceive sensations in these areas. However, dysfunction of the deep perineal nerve may result in altered sensation, numbness, or tingling in the affected areas, warranting further investigation and potential medical intervention.
For example, damage to the deep perineal nerve during childbirth or pelvic surgery can lead to sensory disturbances in the perineum and genital region. Patients may experience a loss of sensation or abnormal sensations, affecting their overall quality of life.
Motor Functions
Motor fibers within the deep perineal nerve control the contraction and relaxation of the external urethral sphincter and associated muscles. These actions contribute to urinary continence and the voluntary regulation of urination.
When the deep perineal nerve is functioning properly, it allows individuals to maintain control over their bladder function. The external urethral sphincter contracts to prevent urine leakage and relaxes when it is time to urinate.
However, dysfunction of the deep perineal nerve can manifest as urinary incontinence or difficulties in initiating or stopping urine flow. This can significantly impact an individual’s daily life, leading to embarrassment, social withdrawal, and a decreased quality of life.
Furthermore, the deep perineal nerve also plays a role in sexual function. It provides innervation to the external genitalia, contributing to the sensations experienced during sexual arousal and orgasm. Dysfunction of this nerve can lead to sexual dysfunction, affecting both physical and emotional well-being.
In conclusion, the deep perineal nerve is a vital component of the peripheral nervous system, serving both sensory and motor functions. Its sensory branches transmit important information from the perineum and external genitals, while its motor fibers control the contraction and relaxation of the external urethral sphincter. Dysfunction of this nerve can lead to sensory disturbances, urinary incontinence, and sexual dysfunction, emphasizing the importance of its proper functioning for overall well-being.
Clinical Significance of the Deep Perineal Nerve
Understanding the clinical significance of the deep perineal nerve is crucial for diagnosing and managing associated disorders.
The deep perineal nerve, also known as the pudendal nerve, plays a vital role in the functioning of the pelvic floor muscles and the genitourinary system. It provides sensory innervation to the perineum, urethra, and external genitalia, as well as motor innervation to the muscles involved in urinary and fecal continence.
Common Disorders and Symptoms
Deep perineal nerve disorders can present with a range of symptoms, including urinary incontinence, sensory disturbances, and sexual dysfunction. Conditions such as pudendal neuralgia, nerve compression syndromes, and trauma can lead to debilitating symptoms that significantly impact an individual’s quality of life.
Pudendal neuralgia is a condition characterized by chronic pain in the perineal area, which can radiate to the buttocks and lower back. It is often described as a burning, shooting, or stabbing pain that worsens with sitting or prolonged standing. In addition to pain, individuals may experience numbness, tingling, or a loss of sensation in the genital area.
Nerve compression syndromes, such as entrapment or compression of the pudendal nerve, can occur due to anatomical abnormalities, inflammation, or trauma. These conditions can cause similar symptoms to pudendal neuralgia, including pain, numbness, and sensory disturbances.
Trauma to the perineum, such as during childbirth or pelvic surgery, can also result in deep perineal nerve damage. This can lead to various symptoms, including urinary and fecal incontinence, as well as sexual dysfunction.
However, it is important to note that these symptoms are nonspecific and can be attributed to various other medical conditions. Therefore, consulting with a healthcare professional is essential for an accurate diagnosis.
Diagnostic Techniques
Diagnosing deep perineal nerve disorders often involves a comprehensive evaluation, including a thorough medical history, physical examination, and, in specific cases, neurophysiological testing.
During the medical history assessment, the healthcare professional will inquire about the nature, duration, and severity of symptoms, as well as any potential triggering factors or previous injuries. They will also ask about the individual’s medical and surgical history, as certain conditions or procedures may increase the risk of deep perineal nerve damage.
A physical examination may involve assessing the pelvic floor muscles for strength, tone, and coordination. The healthcare professional may also perform a sensory examination to evaluate any abnormalities in the perineal area and genitalia. Additionally, a digital rectal examination may be conducted to assess the anal sphincter tone and rule out any associated pathology.
In specific cases, neurophysiological testing may be recommended to further evaluate the function of the deep perineal nerve. Electromyography (EMG) can assess the electrical activity of the muscles innervated by the nerve, while nerve conduction studies can measure the speed and strength of nerve impulses. Imaging techniques, such as magnetic resonance imaging (MRI), may also aid in identifying the underlying cause of symptoms and guide appropriate management strategies.
It is important to consult with a medical professional to determine the most suitable diagnostic approach for individual cases. Early diagnosis and intervention can significantly improve outcomes and help individuals regain their quality of life.
Treatment and Management of Deep Perineal Nerve Disorders
Deep perineal nerve disorders require a multidisciplinary approach for effective treatment and management. These disorders can cause significant discomfort and impact a person’s quality of life. It is important to explore various treatment options to alleviate symptoms and address the underlying causes of the condition.
Non-Surgical Interventions
Non-surgical interventions for deep perineal nerve disorders aim to alleviate symptoms and improve quality of life. Physical therapy plays a crucial role in the management of these disorders. It involves exercises and techniques that help strengthen the pelvic floor muscles and improve nerve function. Pelvic floor exercises, also known as Kegel exercises, can be highly beneficial in reducing pain and improving bladder and bowel control.
Lifestyle modifications are another important aspect of non-surgical interventions. These may include dietary changes, weight management, and avoiding activities that exacerbate symptoms. For some individuals, modifying their daily routine and avoiding prolonged sitting or activities that put pressure on the perineal area can provide significant relief.
Pharmacological interventions can also be used to manage deep perineal nerve disorders. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce pain and inflammation. Neuropathic agents, such as gabapentin or pregabalin, can be prescribed to target nerve-related pain. Muscle relaxants may also be used to alleviate muscle spasms and reduce discomfort.
Complementary therapies, such as acupuncture, have shown promise in providing relief for deep perineal nerve disorders. Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the nervous system and promote healing. Nerve blocks, which involve the injection of anesthetic medication near the affected nerve, can also provide temporary relief from pain and discomfort.
It is important to note that the effectiveness of non-surgical interventions may vary from person to person. Consulting with a healthcare professional experienced in managing deep perineal nerve disorders is crucial to develop an individualized treatment plan that addresses the specific needs and underlying causes of each patient’s condition.
Surgical Procedures
In cases where non-surgical interventions do not provide sufficient relief, surgical interventions may be considered. Surgical procedures for deep perineal nerve disorders are typically reserved for individuals who have not responded to conservative treatments and are experiencing severe and persistent symptoms.
Decompression surgery is one option for relieving nerve compression. This procedure involves removing any structures that may be compressing the affected nerve, such as scar tissue or abnormal growths. By alleviating the pressure on the nerve, decompression surgery aims to restore normal nerve function and reduce pain and other symptoms.
Neurectomy is another surgical procedure that may be performed to treat focal nerve entrapment. It involves the removal of a portion of the affected nerve, which can help alleviate symptoms in some cases. However, neurectomy is considered a last resort and is only recommended when other treatment options have been exhausted.
It is important to emphasize that these surgical interventions should only be pursued after careful consideration, with the guidance of a healthcare professional experienced in managing deep perineal nerve disorders. Surgical procedures carry risks and potential complications, and the decision to undergo surgery should be based on a thorough evaluation of the individual’s condition and the potential benefits and risks of the procedure.
In conclusion, the treatment and management of deep perineal nerve disorders require a comprehensive approach that may involve non-surgical interventions, such as physical therapy, lifestyle modifications, and pharmacological interventions. In cases where these interventions are not effective, surgical procedures may be considered. It is important for individuals with deep perineal nerve disorders to work closely with healthcare professionals to develop a personalized treatment plan that addresses their specific needs and aims to improve their quality of life.
Future Research Directions in Deep Perineal Nerve Study
Ongoing research in the field of deep perineal nerve study is focused on exploring novel therapeutic approaches and answering unanswered questions. The study of the deep perineal nerve plays a vital role in understanding and treating various disorders that affect this important nerve.
The deep perineal nerve is responsible for innervating the muscles and skin in the perineal region, which is located between the anus and the external genitalia. Disorders of this nerve can lead to a variety of symptoms, including pain, numbness, and loss of function in the affected area. Understanding the underlying mechanisms of these disorders is crucial for developing effective treatment strategies.
Emerging Therapies
Advancements in medical technology and understanding of nerve physiology have led to the emergence of innovative therapeutic modalities for deep perineal nerve disorders. These include neuromodulation techniques, regenerative medicine approaches, and minimally invasive procedures. Neuromodulation techniques involve the use of electrical or chemical stimulation to modulate the activity of the deep perineal nerve, providing relief from pain and improving function. Regenerative medicine approaches aim to repair or regenerate damaged nerve tissue using stem cells or other biological materials. Minimally invasive procedures, such as nerve decompression surgery, offer a less invasive alternative to traditional open surgery.
While still in the investigative stage, these emerging therapies hold potential for improving treatment outcomes and enhancing patients’ quality of life. However, further research and clinical trials are necessary to establish their safety and efficacy. Researchers are working diligently to gather evidence and gather data to support the use of these therapies in clinical practice.
Unanswered Questions in Deep Perineal Nerve Research
Despite significant advancements in our understanding of the deep perineal nerve, there are still unanswered questions that warrant further exploration. These areas of research include elucidating the precise mechanisms underlying deep perineal nerve disorders, identifying potential risk factors, refining diagnostic techniques, and developing more targeted and personalized treatment options.
Researchers are actively investigating the cellular and molecular mechanisms that contribute to deep perineal nerve disorders. By understanding these mechanisms, they hope to develop targeted therapies that can specifically address the underlying causes of these disorders. Additionally, identifying potential risk factors for deep perineal nerve disorders can help healthcare providers identify individuals who may be at a higher risk and implement preventive measures.
Refining diagnostic techniques is another important area of research in deep perineal nerve study. Accurate and early diagnosis is crucial for providing timely treatment and improving patient outcomes. Researchers are exploring new imaging modalities, such as magnetic resonance imaging (MRI) and ultrasound, to improve the visualization of the deep perineal nerve and aid in diagnosis.
Furthermore, the development of more targeted and personalized treatment options is a priority in deep perineal nerve research. Each patient’s condition is unique, and tailoring treatment approaches to individual needs can lead to better outcomes. Researchers are investigating the use of biomarkers and genetic profiling to identify specific subtypes of deep perineal nerve disorders and develop personalized treatment plans.
Continued collaboration among researchers, clinicians, and patients will be crucial for advancing our knowledge in this field. By working together, they can share insights, exchange ideas, and conduct large-scale studies to further our understanding of deep perineal nerve disorders and improve patient care.
Conclusion
Understanding the role of the deep perineal nerve is essential for comprehending the complexities associated with deep perineal nerve disorders. This comprehensive guide has provided a detailed overview of the anatomy, physiological role, clinical significance, and treatment options related to the deep perineal nerve. By recognizing the importance of multidisciplinary management and staying informed about emerging therapies and research trends, healthcare professionals can provide optimal care for individuals affected by deep perineal nerve disorders. Early diagnosis, individualized treatment plans, and ongoing research efforts are key to improving outcomes and enhancing patient well-being.