In this article, we will delve into the topic of perineal nerve compression—a condition that can cause significant discomfort and disrupt daily life. We will explore the various causes, symptoms, diagnostic procedures, treatment options, and prevention strategies associated with this condition.
What is Perineal Nerve Compression?
The perineal nerve is a branch of the pudendal nerve, which originates from the sacral plexus. It supplies sensation to the perineum—the area between the anus and the genitals—and the surrounding muscles. Perineal nerve compression occurs when this nerve is compressed or damaged, leading to a variety of symptoms.
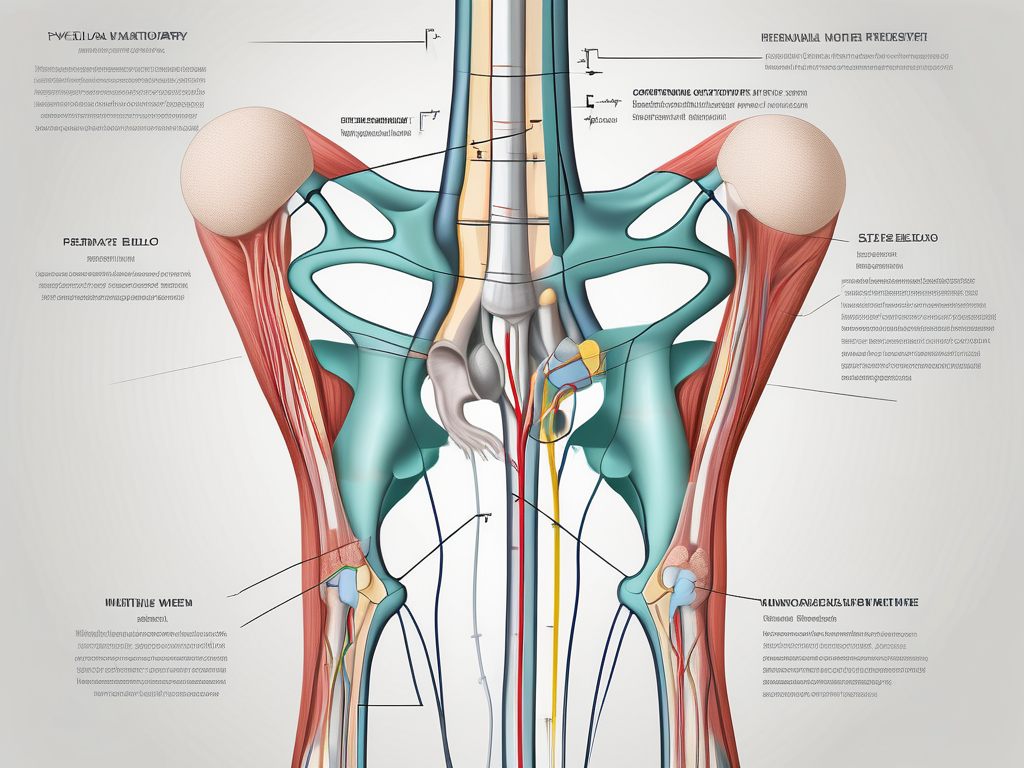
The Anatomy of the Perineal Nerve
To understand the impact of perineal nerve compression, it is crucial to familiarize ourselves with its intricate anatomy. The perineal nerve arises from the S2-S4 spinal nerves and travels through the pelvis, branching into several smaller nerves that innervate different areas within the perineum.
The perineal nerve, also known as the inferior pudendal nerve, is one of the main branches of the pudendal nerve. It originates from the sacral plexus, a network of nerves formed by the ventral rami of the sacral spinal nerves. The perineal nerve emerges from the pelvis through the greater sciatic foramen, passing below the piriformis muscle.
As it continues its course, the perineal nerve gives off branches that supply sensation to various structures in the perineum. These branches include the posterior scrotal nerves in males and the posterior labial nerves in females, which provide sensation to the skin of the scrotum and labia majora, respectively. The perineal nerve also innervates the muscles of the perineum, such as the external anal sphincter and the bulbospongiosus muscle.
The Role of the Perineal Nerve in the Body
The perineal nerve plays a pivotal role in both sensory and motor functions. It provides sensation to the perineum, including the genital area, and contributes to the control of muscles involved in urinary and bowel functions.
When it comes to sensory functions, the perineal nerve carries sensory information from the perineum to the brain. This includes sensations of touch, pressure, temperature, and pain. Without the perineal nerve, the perineum would lose its ability to perceive these sensations, leading to a significant impairment in daily activities and overall quality of life.
Motor functions involve the control of muscles. The perineal nerve innervates the external anal sphincter, which is responsible for maintaining continence and controlling the release of feces. It also supplies the bulbospongiosus muscle, which plays a role in sexual functions, such as erection and ejaculation in males, and clitoral erection in females.
In addition to its role in bowel and sexual functions, the perineal nerve contributes to the coordination of pelvic floor muscles. These muscles are essential for maintaining pelvic organ support and preventing conditions such as pelvic organ prolapse. The perineal nerve ensures the proper functioning of these muscles, allowing for optimal pelvic floor control and stability.
Overall, the perineal nerve is a vital component of the nervous system, playing a crucial role in both sensory and motor functions. When compressed or damaged, it can lead to a range of symptoms and impairments that significantly impact a person’s daily life. Understanding the anatomy and function of the perineal nerve is essential in diagnosing and managing perineal nerve compression effectively.
Causes of Perineal Nerve Compression
Several factors can contribute to perineal nerve compression. Understanding these causes is crucial in determining appropriate treatment strategies.
Perineal nerve compression occurs when the perineal nerve, which is responsible for providing sensation to the perineum and controlling the muscles in that area, becomes compressed or damaged. This compression can result in a variety of symptoms, including pain, numbness, and tingling.
Physical Trauma and Injuries
One common cause of perineal nerve compression is physical trauma or injuries to the pelvic region. Accidents, falls, or sports-related injuries can lead to nerve damage or compression, resulting in symptoms such as pain, numbness, and tingling.
For example, a fall from a bike or a direct blow to the pelvic area during contact sports can cause significant trauma to the perineum, leading to nerve compression. In some cases, the compression may be temporary and resolve on its own with rest and conservative treatment. However, severe trauma or repeated injuries may require more extensive medical intervention.
Medical Conditions Leading to Nerve Compression
Several medical conditions can contribute to perineal nerve compression. These include herniated discs, pelvic tumors, pelvic inflammatory disease, and infections. It is important to note that any condition that causes inflammation or swelling in the pelvic region can potentially impact the perineal nerve.
For instance, a herniated disc in the lumbar spine can put pressure on the nerves that travel down to the perineum, leading to compression. Similarly, pelvic tumors can grow and exert pressure on the perineal nerve, causing compression and subsequent symptoms. Infections, such as urinary tract infections or sexually transmitted infections, can also lead to inflammation in the pelvic region, potentially affecting the perineal nerve.
Lifestyle Factors Contributing to Perineal Nerve Compression
Additionally, certain lifestyle factors can increase the risk of perineal nerve compression. Prolonged sitting, especially on hard surfaces, can exert pressure on the perineum, potentially compressing the nerve. Obesity and poor posture can also contribute to the development of this condition.
Individuals who spend long hours sitting at a desk or driving for extended periods may be at a higher risk of developing perineal nerve compression. The constant pressure on the perineum can gradually lead to nerve compression over time. Similarly, obesity can put extra weight on the pelvic area, increasing the likelihood of nerve compression. Poor posture, such as slouching or hunching, can also contribute to the compression of the perineal nerve.
It is important to address these lifestyle factors to prevent or alleviate perineal nerve compression. Making ergonomic adjustments to seating arrangements, maintaining a healthy weight through regular exercise and a balanced diet, and practicing good posture can all help reduce the risk of nerve compression in the perineum.
Recognizing the Symptoms of Perineal Nerve Compression
Identifying the symptoms of perineal nerve compression is crucial for prompt intervention and management. Early recognition can prevent further damage and improve outcomes.
Perineal nerve compression occurs when there is pressure or irritation on the perineal nerve, which is responsible for providing sensation and controlling the muscles in the perineal region. This compression can be caused by various factors, such as trauma, inflammation, or compression from surrounding structures.
Understanding the symptoms associated with perineal nerve compression is essential for early detection and appropriate treatment. By recognizing these symptoms, individuals can seek medical attention and receive timely intervention.
Early Warning Signs
Early symptoms of perineal nerve compression may include mild discomfort, numbness, or tingling in the perineal region. These sensations may be intermittent or persistent, depending on the severity of the compression.
Individuals experiencing perineal nerve compression may also notice a sensation of weakness or difficulty controlling the pelvic muscles. This can manifest as difficulty with activities such as walking, sitting, or maintaining bladder or bowel control.
It is important to note that these early warning signs can vary in intensity and may be mistaken for other conditions. Therefore, it is crucial to consult with a healthcare professional for a proper diagnosis and appropriate management.
Progression of Symptoms
If left untreated, perineal nerve compression can lead to worsening symptoms and potentially impact an individual’s quality of life. As the compression persists, individuals may experience chronic pain in the perineal region, which can be debilitating and affect daily activities.
Persistent numbness or tingling in the perineal area can also develop as the compression continues. This can lead to a loss of sensation, making it difficult to detect temperature changes or perceive touch accurately.
In addition to sensory changes, muscle weakness may become more pronounced over time. This can result in difficulties with coordination and controlling the pelvic muscles, leading to problems with urination or bowel movements.
Recognizing the progression of symptoms is crucial for seeking appropriate medical attention and intervention. Early treatment can help alleviate symptoms and prevent further nerve damage.
When to Seek Medical Attention
If you experience any persistent or worsening symptoms associated with perineal nerve compression, it is crucial to seek medical attention. A healthcare professional, such as a neurologist or urologist, can conduct a thorough evaluation and determine an appropriate course of action.
During the evaluation, the healthcare professional may perform a physical examination, review medical history, and order diagnostic tests such as nerve conduction studies or imaging scans. These tests can help identify the underlying cause of the nerve compression and guide treatment decisions.
Early intervention is key in managing perineal nerve compression effectively. Treatment options may include physical therapy, medication to alleviate pain and inflammation, or, in severe cases, surgical intervention to relieve the compression on the nerve.
Remember, seeking medical attention promptly can lead to better outcomes and improve your overall quality of life.
Diagnostic Procedures for Perineal Nerve Compression
Diagnosing perineal nerve compression involves a multidimensional approach, including physical examinations, imaging tests, and specialized nerve conduction studies.
Perineal nerve compression can cause a variety of symptoms, such as pain, numbness, tingling, or muscle weakness in the perineal region. To accurately diagnose this condition, healthcare providers employ a combination of diagnostic procedures to gather comprehensive information about the patient’s condition.
Physical Examination
During a physical examination, your healthcare provider will assess the perineal region for signs of inflammation, tenderness, or muscle weakness. They may also perform various provocative tests to evaluate nerve function.
The physical examination begins with a thorough inspection of the perineal area. The healthcare provider carefully examines the skin for any visible abnormalities, such as redness, swelling, or rashes. They also palpate the area, applying gentle pressure to identify any areas of tenderness or discomfort.
In addition to the visual and tactile examination, the healthcare provider may also assess muscle strength and coordination in the perineal region. They may ask the patient to perform specific movements or exercises to evaluate the function of the muscles innervated by the perineal nerve.
Furthermore, the healthcare provider may perform provocative tests to elicit specific symptoms or reproduce the patient’s pain. These tests can help determine the exact location and severity of the nerve compression.
Imaging Tests
In some cases, imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used to visualize the pelvic region. These tests help identify any structural abnormalities or signs of nerve compression.
MRI is a non-invasive imaging technique that uses powerful magnets and radio waves to create detailed images of the internal structures of the body. It can provide high-resolution images of the perineal region, allowing healthcare providers to identify any anatomical abnormalities, such as herniated discs, tumors, or cysts that may be compressing the perineal nerve.
CT scans, on the other hand, use a combination of X-rays and computer technology to create cross-sectional images of the body. This imaging modality can provide detailed information about the bones, muscles, and other structures in the pelvic region, helping healthcare providers identify any potential sources of nerve compression.
Electromyography and Nerve Conduction Studies
Electromyography (EMG) and nerve conduction studies (NCS) are specialized tests that assess the function of nerves and muscles. These tests can provide valuable information about the extent and location of nerve compression.
During an EMG, a small needle electrode is inserted into the muscles of the perineal region. The electrode records the electrical activity of the muscles at rest and during contraction. This information helps healthcare providers evaluate the integrity of the perineal nerve and the associated muscles.
NCS, on the other hand, involves the application of small electrical shocks to the perineal nerve. The healthcare provider measures the speed and strength of the nerve’s response, providing information about its conduction ability. Abnormalities in nerve conduction can indicate the presence of nerve compression.
By combining the results of the physical examination, imaging tests, and specialized nerve conduction studies, healthcare providers can accurately diagnose perineal nerve compression and develop an appropriate treatment plan tailored to the individual needs of the patient.
Treatment Options for Perineal Nerve Compression
The management of perineal nerve compression typically involves a combination of non-surgical treatments, surgical interventions, and rehabilitation strategies.
Perineal nerve compression occurs when there is pressure or damage to the perineal nerve, which is responsible for providing sensation and motor function to the perineal region. This compression can result in symptoms such as pain, numbness, tingling, and weakness in the affected area.
Non-Surgical Treatments
Conservative approaches, such as physical therapy, pain management techniques, and lifestyle modifications, are often the initial steps in treatment. Physical therapy can help strengthen the muscles surrounding the perineal region, improve blood flow, and promote healing. Pain management techniques, such as medications, nerve blocks, and transcutaneous electrical nerve stimulation (TENS), aim to alleviate discomfort and improve overall well-being.
In addition to physical therapy and pain management, lifestyle modifications can also play a significant role in managing perineal nerve compression. These modifications may include avoiding activities that exacerbate symptoms, maintaining a healthy weight, and practicing good posture.
Surgical Interventions
In cases where conservative treatments have not provided sufficient relief, surgical interventions may be considered. The specific surgical procedure will depend on the underlying cause of the perineal nerve compression. Common surgical interventions include decompression surgery, where the pressure on the nerve is relieved by removing or repositioning surrounding structures, and nerve repair or grafting, where damaged sections of the nerve are repaired or replaced.
It is important to note that surgical interventions carry their own risks and potential complications, and the decision to undergo surgery should be made in consultation with a qualified healthcare professional.
Rehabilitation and Recovery Process
Following surgery or during the non-surgical treatment phase, rehabilitation plays a crucial role in the recovery process. Physical therapy and targeted exercises can assist in restoring muscle strength, improving mobility, and enhancing overall quality of life.
Rehabilitation programs may include a combination of exercises to strengthen the perineal muscles, improve coordination and balance, and enhance flexibility. Additionally, techniques such as manual therapy, massage, and stretching may be utilized to alleviate muscle tension and promote healing.
Recovery from perineal nerve compression can vary depending on the severity of the condition and the individual’s response to treatment. It is important to follow the guidance of healthcare professionals and adhere to the prescribed rehabilitation program to optimize the chances of a successful recovery.
In conclusion, the management of perineal nerve compression involves a comprehensive approach that includes non-surgical treatments, surgical interventions, and rehabilitation strategies. By combining these approaches, healthcare professionals aim to alleviate symptoms, restore normal nerve function, and improve the overall well-being of individuals affected by perineal nerve compression.
Prevention Strategies for Perineal Nerve Compression
While it may not always be possible to prevent perineal nerve compression, certain strategies can help reduce the risk or minimize its impact.
Lifestyle Modifications
Sustaining good posture, avoiding prolonged periods of sitting on hard surfaces, and taking regular breaks during sedentary activities can help reduce the risk of perineal nerve compression. Maintaining a healthy weight and addressing any underlying medical conditions promptly are also important preventive measures.
Regular Exercise and Stretching
Engaging in regular physical activity and incorporating stretching exercises can improve muscle strength, flexibility, and overall pelvic health. Consult with a healthcare professional or a certified exercise specialist for tailored exercise recommendations.
Importance of Early Diagnosis and Treatment
Early diagnosis and treatment play a key role in preventing the progression of perineal nerve compression. If you experience any symptoms or have concerns, it is important to consult with a healthcare professional for a comprehensive evaluation and appropriate management.
Conclusion
Understanding the causes, symptoms, diagnostic procedures, treatment options, and prevention strategies associated with perineal nerve compression is essential for comprehensive management. By familiarizing ourselves with this condition and seeking timely medical attention, we can strive for optimal outcomes and improve overall quality of life.