The perineal nerve is a vital part of the female anatomy. Understanding its anatomy, function, and potential disorders associated with it is key to maintaining overall well-being and quality of life. In this comprehensive guide, we will explore the intricacies of the perineal nerve, its role in sensation and function, disorders related to it, available treatment options, prevention and management strategies, and the impact of perineal nerve disorders on a woman’s quality of life.
Anatomy of the Perineal Nerve
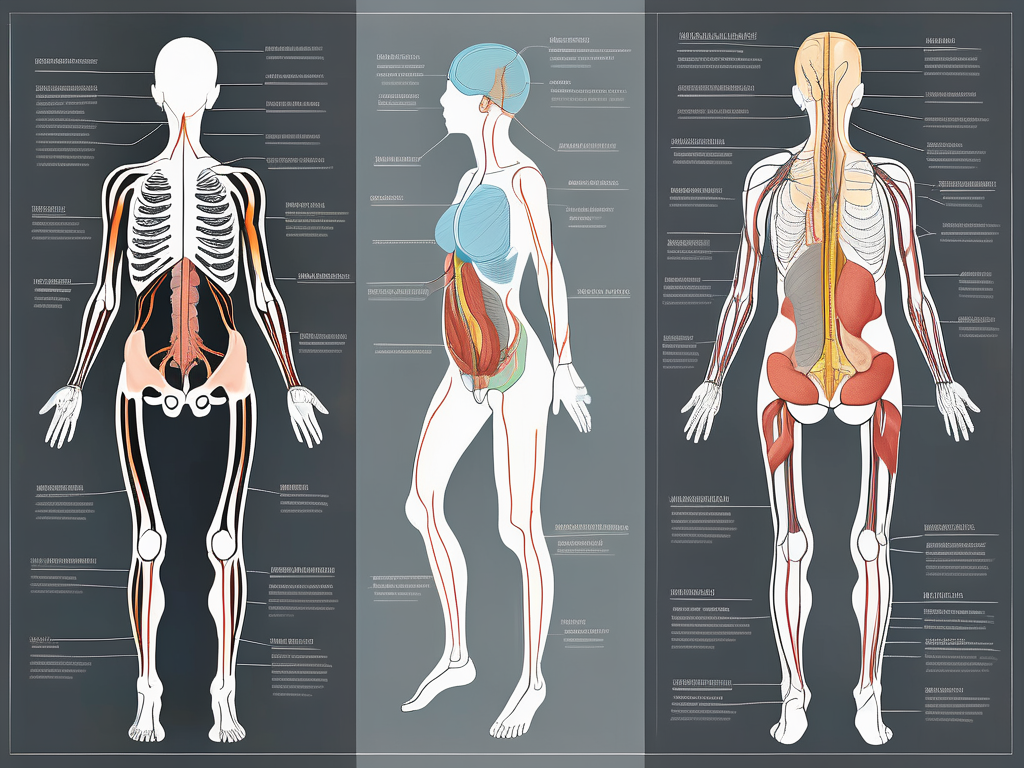
Before delving into the specifics, it is important to grasp the basic anatomy of the perineal nerve. The perineal nerve is a branch of the pudendal nerve system, which originates from the sacral plexus. The sacral plexus is a complex network of nerves formed by the fusion of the anterior rami of the spinal nerves S1 to S4. This intricate web of nerves serves as a vital communication pathway between the central nervous system and the perineal region.
The perineal nerve, as part of the pudendal nerve system, travels through the perineum, the area between the vagina and anus. This region is often referred to as the “diamond-shaped” area, as it is bounded by the pubic symphysis anteriorly, the coccyx posteriorly, and the ischial tuberosities laterally. The perineal nerve provides innervation to the external genitalia, perineal muscles, and skin of the anal region.
Within the perineum, the perineal nerve branches out to supply various structures. It sends branches to the labia majora and minora in females and the scrotum and penis in males. These branches ensure the proper sensory feedback from the external genitalia, allowing for sexual pleasure and facilitating the coordination of pelvic floor muscles during sexual intercourse.
In addition to its role in sexual function, the perineal nerve also plays a crucial role in the control of bowel and bladder movements. It provides sensory feedback from the anal region, allowing for the perception of rectal distension and the initiation of defecation. The perineal nerve also innervates the external anal sphincter, a muscle responsible for maintaining continence and controlling the release of stool.
The Perineal Nerve and the Pudendal Nerve System
The perineal nerve works in conjunction with the pudendal nerve system to ensure proper sensory and motor function in the pelvic area. The pudendal nerve system encompasses three main nerves – the perineal nerve, the inferior rectal nerve, and the dorsal nerve of the clitoris in females or the dorsal nerve of the penis in males. Each of these nerves serves a distinct area of the perineal region, forming a complex network that enables normal urinary, sexual, and bowel function.
The inferior rectal nerve, a branch of the pudendal nerve system, supplies the external anal sphincter and the perianal skin. It plays a crucial role in maintaining continence and providing sensation to the anal region.
The dorsal nerve of the clitoris in females or the dorsal nerve of the penis in males is responsible for providing sensory innervation to the clitoris or penis, respectively. This nerve is essential for sexual pleasure and arousal.
Together, the perineal nerve, the inferior rectal nerve, and the dorsal nerve of the clitoris or penis form a comprehensive network that ensures the proper functioning of the perineal region. Any disruption in this intricate system can lead to various disorders, such as sexual dysfunction, urinary incontinence, or fecal incontinence.
The Role of the Perineal Nerve in Sensation and Function
The perineal nerve plays a crucial role in both sensation and function. It provides sensory feedback from the external genitalia, enabling sexual pleasure and facilitating the coordination of pelvic floor muscles during sexual intercourse. The intricate network of nerves within the perineum allows for precise sensation and control in the pelvic region, contributing to a fulfilling sexual experience.
In addition to its role in sexual function, the perineal nerve aids in the control of bowel and bladder movements. It provides sensory feedback from the anal region, allowing for the perception of rectal distension and the initiation of defecation. The perineal nerve also innervates the external anal sphincter, a muscle responsible for maintaining continence and controlling the release of stool.
Disorders affecting the perineal nerve can have significant implications on an individual’s quality of life. Damage to the perineal nerve can result from trauma, compression, or disease processes. Common symptoms of perineal nerve dysfunction include numbness or tingling in the perineal region, pain during sexual intercourse, urinary or fecal incontinence, and difficulty with bowel movements.
In conclusion, the perineal nerve is a vital component of the pudendal nerve system, playing a crucial role in both sensation and function. Its intricate network of branches ensures proper innervation to the external genitalia, perineal muscles, and anal region. Understanding the anatomy and function of the perineal nerve is essential for diagnosing and managing disorders affecting the perineal region.
Disorders Related to the Perineal Nerve
Perineal nerve disorders can arise from a variety of causes. Damage to the nerve can result from childbirth trauma, surgical procedures in the pelvic region, infections, or prolonged pressure on the nerve. It is important to note that while perineal nerve disorders predominantly affect women, men can also experience similar conditions involving the perineal nerve.
The perineal nerve, also known as the pudendal nerve, is a crucial component of the pelvic region. It provides sensory and motor innervation to the perineum, which includes the area between the genitals and the anus. Any disruption or damage to this nerve can have a significant impact on a person’s quality of life.
Causes of Perineal Nerve Damage
There are several factors that can contribute to perineal nerve damage. Childbirth presents a significant risk, particularly if assisted delivery techniques are required or if the birth involves a prolonged second stage. The pressure exerted on the nerve during childbirth can lead to stretching or compression, resulting in injury. In some cases, the use of forceps or vacuum extraction can also cause direct trauma to the nerve.
Surgical procedures such as pelvic surgeries or episiotomies can also result in nerve damage. During these procedures, the perineal nerve may be inadvertently injured or compressed, leading to symptoms of perineal nerve disorders. Infections, such as herpes or urinary tract infections, can affect the perineal nerve as well. The inflammatory response triggered by these infections can irritate the nerve and disrupt its normal functioning.
Additionally, prolonged pressure on the nerve, such as sitting in one position for extended periods, can lead to damage over time. Occupations or activities that require prolonged sitting, such as truck driving or cycling, can increase the risk of perineal nerve disorders. The constant pressure on the nerve can impede blood flow and cause nerve compression, resulting in symptoms such as pain, numbness, or tingling in the perineal region.
Symptoms and Diagnosis of Perineal Nerve Disorders
The symptoms of perineal nerve disorders can vary depending on the extent and location of the nerve damage. Common symptoms include pain or numbness in the perineal region, difficulty controlling bowel or bladder function, sexual dysfunction, and pelvic floor muscle weakness. These symptoms can significantly impact a person’s daily activities and overall well-being.
A thorough medical evaluation is necessary to diagnose perineal nerve disorders. It typically involves a detailed history, physical examination, and potentially diagnostic tests such as electromyography. Electromyography measures the electrical activity of muscles and can help identify any abnormalities or nerve damage. Consulting with a healthcare professional who specializes in pelvic pain or neurology is crucial in order to receive an accurate diagnosis and appropriate treatment plan.
Treatment options for perineal nerve disorders may include a combination of medication, physical therapy, and lifestyle modifications. Medications such as pain relievers or nerve-specific medications can help manage symptoms. Physical therapy techniques, such as pelvic floor exercises or nerve mobilization, can improve muscle strength and reduce pain. Lifestyle modifications, such as avoiding activities that exacerbate symptoms or using cushions to relieve pressure on the perineal region, may also be recommended.
It is important to seek timely medical attention if you suspect you may be experiencing symptoms related to perineal nerve disorders. Early diagnosis and intervention can lead to better outcomes and improved quality of life.
Treatment Options for Perineal Nerve Disorders
Perineal nerve disorders can be debilitating and affect the quality of life for individuals experiencing them. Fortunately, there are treatment options available to help manage and alleviate the symptoms associated with these disorders. The choice of treatment depends on various factors, including the underlying cause, severity of symptoms, and individual needs.
Non-surgical treatments and therapies are often the first-line approach in managing perineal nerve disorders. These treatments focus on symptom management and improving nerve function. One common non-surgical treatment option is pain management techniques, which may include the use of medications, nerve blocks, or alternative therapies such as acupuncture. These techniques aim to reduce pain and discomfort caused by the nerve disorder.
In addition to pain management, physical therapy is another important aspect of non-surgical treatment for perineal nerve disorders. Physical therapy aims to strengthen the pelvic floor muscles, which can help improve bladder and bowel control. This may involve exercises specifically designed to target the muscles in the perineal area, as well as techniques to improve overall muscle coordination and control.
Specialized devices can also be used as part of non-surgical treatment for perineal nerve disorders. These devices are designed to improve bladder or bowel control and can include items such as catheters, pessaries, or electrical stimulation devices. These devices work by providing support or stimulating the nerves in the perineal area, helping to restore normal function and control.
It is important for individuals with perineal nerve disorders to work closely with a healthcare professional to develop a tailored treatment plan that best suits their specific needs. This may involve a combination of non-surgical treatments and therapies, depending on the severity of symptoms and individual circumstances.
Surgical Interventions for Perineal Nerve Damage
In some cases, non-surgical treatments may be insufficient or ineffective in managing perineal nerve disorders. In these situations, surgical interventions may be considered as a last resort. Surgical options for perineal nerve damage can vary depending on the cause and extent of the nerve damage.
Nerve decompression or repair procedures are commonly performed surgical interventions for perineal nerve disorders. These procedures aim to relieve pressure on the affected nerve or repair any damage that may be present. Nerve decompression involves removing any structures or tissues that may be compressing the nerve, while nerve repair procedures aim to reconnect or regenerate damaged nerve fibers.
In more severe cases, nerve grafts may be necessary to restore nerve function. Nerve grafting involves taking a healthy nerve from another part of the body and transplanting it to the damaged area. This procedure allows for the regeneration of nerve fibers and can help restore sensation and function in the perineal region.
Another surgical intervention that may be considered for perineal nerve disorders is neuromodulation. This technique involves the implantation of a device that delivers electrical impulses to the affected nerves, helping to regulate their activity and alleviate symptoms. Neuromodulation can be an effective option for individuals who have not responded well to other treatments.
It is crucial for individuals considering surgical interventions for perineal nerve disorders to thoroughly discuss the risks, benefits, and potential outcomes with a qualified healthcare professional. This will ensure that informed decisions are made regarding the most appropriate surgical approach for each individual case.
Prevention and Management of Perineal Nerve Disorders
While not all perineal nerve disorders are preventable, there are steps that can be taken to minimize the risk of damage or manage existing conditions effectively.
Perineal nerve disorders can have a significant impact on an individual’s quality of life. These disorders can cause symptoms such as pain, numbness, tingling, and loss of bladder or bowel control. However, with proper prevention and management strategies, individuals can reduce the risk of developing these conditions or effectively manage existing ones.
Lifestyle Changes for Perineal Nerve Health
Adopting a healthy lifestyle can positively impact perineal nerve health. Maintaining a balanced diet rich in nutrients, vitamins, and minerals is essential for overall nerve health. Including foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats can provide the necessary nutrients to support nerve function and reduce the risk of damage.
In addition to a healthy diet, regular physical activity is crucial for maintaining optimal perineal nerve health. Engaging in exercises that promote blood circulation to the perineal region, such as walking, swimming, or cycling, can help nourish the nerves and prevent compression or damage. It is important to avoid prolonged pressure on the perineal region, especially during activities such as sitting for long periods or cycling on hard surfaces. Taking breaks, using cushioned seats, or using ergonomic equipment can help reduce the risk of nerve compression.
Managing stress levels is also vital for perineal nerve health. Chronic stress can contribute to muscle tension and inflammation, which can affect nerve function. Incorporating stress management techniques such as meditation, deep breathing exercises, or engaging in hobbies and activities that promote relaxation can help reduce stress and support overall nerve health.
Practicing good hygiene is another important aspect of perineal nerve health. Maintaining proper cleanliness in the perineal area can help prevent infections and reduce the risk of nerve damage. Using mild, pH-balanced cleansers and avoiding harsh chemicals or irritants can help maintain the natural balance of the perineal region and protect the nerves.
Exercises to Strengthen the Perineal Nerve
Specific exercises targeting the perineal region can help strengthen the muscles and improve nerve function. Pelvic floor exercises, such as Kegels, are commonly recommended to enhance perineal muscle tone and improve bladder and bowel control. These exercises involve contracting and relaxing the muscles of the pelvic floor, which includes the perineal region.
Consulting with a healthcare professional, such as a physical therapist specializing in pelvic floor health, can provide guidance on appropriate exercises tailored to individual needs. They can assess the strength and function of the perineal muscles and design a personalized exercise program to address specific concerns.
In addition to pelvic floor exercises, other activities such as yoga or Pilates can also help strengthen the perineal muscles and improve nerve function. These exercises focus on core strength and stability, which can indirectly benefit the perineal region.
It is important to note that consistency and proper technique are key when performing exercises to strengthen the perineal nerve. Starting with gentle exercises and gradually increasing intensity and duration can help prevent muscle strain or injury.
In conclusion, preventing and managing perineal nerve disorders requires a holistic approach that includes adopting a healthy lifestyle, practicing good hygiene, and engaging in targeted exercises. By taking proactive steps to support perineal nerve health, individuals can reduce the risk of developing these disorders or effectively manage existing conditions.
The Impact of Perineal Nerve Disorders on Quality of Life
Beyond the physical symptoms, perineal nerve disorders can have a significant impact on a woman’s quality of life, both emotionally and psychologically.
Emotional and Psychological Effects of Perineal Nerve Disorders
Living with perineal nerve disorders can lead to emotional distress, anxiety, and feelings of isolation. The impact on sexual functioning and intimacy can contribute to decreased self-esteem and strained relationships. It is important to recognize these emotional and psychological effects and seek appropriate support from healthcare professionals, support groups, or therapists specializing in sexual health and relationship counseling.
Coping Strategies for Living with Perineal Nerve Disorders
Developing effective coping strategies can help individuals manage the challenges associated with perineal nerve disorders. Seeking support from family, friends, or support groups can provide a sense of understanding and connection. Additionally, engaging in stress management techniques, exploring alternative therapies such as acupuncture or mindfulness practices, and maintaining open communication with healthcare providers are all essential components of a comprehensive coping strategy.
In conclusion, understanding the perineal nerve in females is crucial for maintaining optimal pelvic health. By familiarizing ourselves with its anatomy, functions, potential disorders, treatment options, prevention strategies, and the impact on quality of life, we can better navigate the complex landscape of perineal nerve health. It is important to consult with a healthcare professional for personalized advice and guidance. Together, we can strive for a comprehensive approach to perineal nerve well-being, ensuring a higher quality of life for women everywhere.