The perineal nerve is a crucial structure within the human body’s nervous system, playing a significant role in both sensory and motor functions. Its distribution and functions are essential to understand, particularly in the context of disorders associated with the perineal nerve. This comprehensive overview aims to provide a detailed exploration of the anatomy, role, disorders, treatment, and future research directions pertaining to the perineal nerve. While this article aims to offer valuable insights, it is important to consult with a medical professional for accurate diagnosis and personalized advice.
Anatomy of the Perineal Nerve
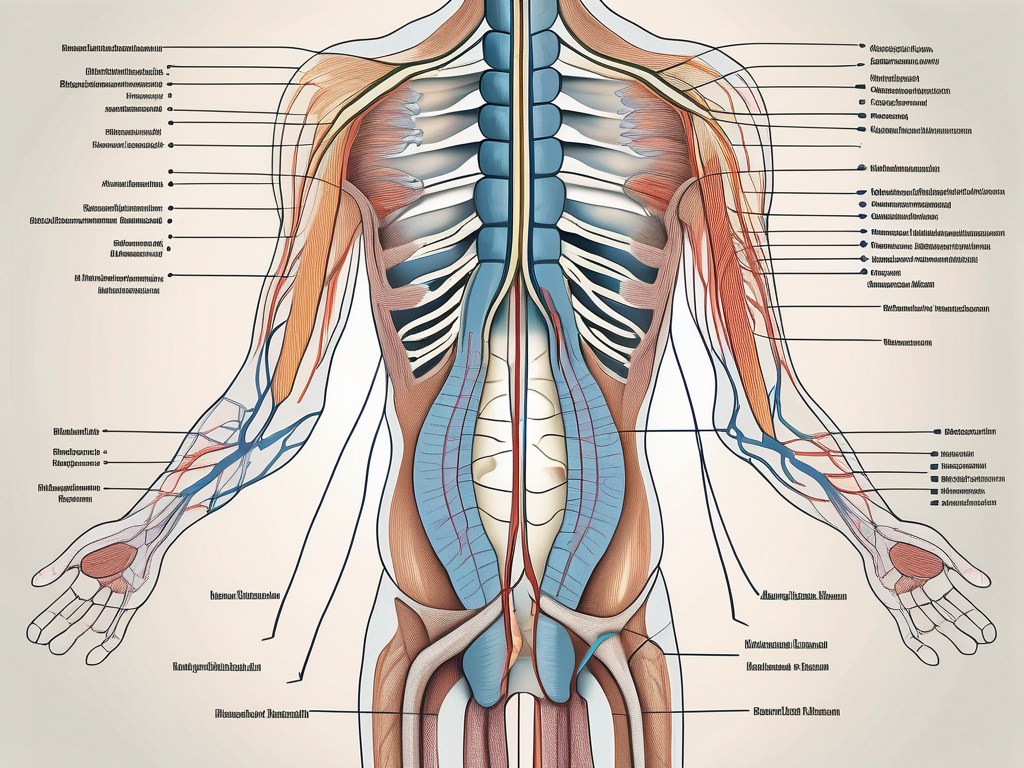
The perineal nerve is a branch of the sacral plexus, arising from the second, third, and fourth sacral nerves. It originates from the ventral rami of these spinal nerves, descends through the greater sciatic foramen, and then enters the perineum through the lesser sciatic foramen. The nerve eventually divides into several branches, each with its own specific function.
Origin and Pathway of the Perineal Nerve
The perineal nerve originates from the sacral plexus, a network of nerves arising from the spinal cord. It carries signals from the sacral region down towards the perineum, which is the anatomical region between the anus and the genitalia. This pathway is of critical importance, as it enables the nerve to provide sensory and motor functions to the perineum and its surrounding structures.
As the perineal nerve descends through the greater sciatic foramen, it traverses through a complex network of muscles and connective tissues. It weaves its way past the piriformis muscle, a deep muscle located in the buttock region. This muscle plays a crucial role in stabilizing the hip joint and aiding in the rotation of the thigh. The perineal nerve’s close proximity to the piriformis muscle highlights the intricate relationship between the nervous and musculoskeletal systems.
Upon entering the perineum through the lesser sciatic foramen, the perineal nerve encounters a rich array of structures. It passes through the ischioanal fossa, a space filled with fat and connective tissue that provides cushioning and support to the surrounding organs. Within this fossa, the nerve interacts with the internal pudendal artery and vein, which supply blood to the perineum and its associated structures.
Branches of the Perineal Nerve
Once the perineal nerve reaches the perineum, it branches into several smaller nerves that innervate specific areas. These branches include the posterior scrotal nerves in males and the posterior labial nerves in females, which supply the skin of the scrotum and labia respectively. These sensory branches play a vital role in transmitting touch, temperature, and pain sensations from the perineum to the central nervous system.
In addition to sensory functions, the perineal nerve also provides innervation to the perineal muscles involved in urinary and bowel control. These muscles, known as the external anal sphincter and the bulbospongiosus muscle, are responsible for maintaining continence and facilitating the expulsion of waste products from the body. The perineal nerve’s motor branches ensure the proper functioning of these muscles, allowing for the coordination of urination and defecation.
Furthermore, the perineal nerve communicates with other nerves in the pelvic region, forming a complex network known as the pelvic plexus. This plexus integrates signals from various sources, including the perineal nerve, to regulate sexual function and reproductive processes. It plays a crucial role in the coordination of sexual arousal, erection, and orgasm, highlighting the intricate interplay between the perineal nerve and the reproductive system.
In summary, the perineal nerve is a vital component of the sacral plexus, providing sensory and motor functions to the perineum and its surrounding structures. Its intricate pathway through the greater and lesser sciatic foramina, as well as its branches to the scrotum/labia and perineal muscles, highlight the complexity and importance of this nerve in maintaining proper bodily function.
The Role of the Perineal Nerve in the Human Body
The perineal nerve serves a dual role in the human body, encompassing both sensory and motor functions. Understanding these functions is crucial in comprehending the impact of disorders associated with the perineal nerve.
The perineal nerve, also known as the pudendal nerve, is a branch of the sacral plexus, originating from the second, third, and fourth sacral spinal nerves. It travels through the pelvis, passing between the piriformis and coccygeus muscles, before reaching the perineum. This nerve is responsible for innervating various structures in the perineal region, playing a vital role in maintaining normal bodily functions.
Sensory Functions of the Perineal Nerve
The perineal nerve is responsible for the sensation in the perineal region, including the anus, perineal skin, and external genitalia. It plays a vital role in conveying various sensory inputs, such as touch, temperature, and pressure, to the central nervous system.
When the perineal nerve detects a stimulus, it sends electrical signals to the brain, allowing us to perceive sensations in the perineal area. For example, when sitting on a chair, the perineal nerve helps us feel the pressure exerted on the skin, ensuring that we can adjust our position to avoid discomfort or pressure sores.
In addition to touch and pressure, the perineal nerve also contributes to the sense of temperature in the perineal region. It enables us to differentiate between hot and cold stimuli, allowing us to respond appropriately to changes in temperature.
Dysfunction of the perineal nerve can lead to altered sensation in these areas, potentially causing discomfort or difficulty in everyday activities. For instance, individuals with perineal nerve damage may experience numbness, tingling, or hypersensitivity in the perineal region, making it challenging to sit for prolonged periods or engage in sexual activities.
Motor Functions of the Perineal Nerve
Aside from sensory functions, the perineal nerve also controls several important motor functions. It supplies the muscles that control urinary and bowel continence, enabling voluntary control over these essential bodily functions.
The perineal nerve innervates the external urethral sphincter, a muscle responsible for maintaining urinary continence. When the perineal nerve receives signals from the brain, it stimulates the external urethral sphincter to contract, preventing the involuntary release of urine. This allows us to control the timing and flow of urination, ensuring proper bladder emptying without leakage.
In addition to urinary continence, the perineal nerve also plays a crucial role in bowel continence. It innervates the external anal sphincter, a muscle that keeps the anal canal closed to prevent involuntary bowel movements. By contracting the external anal sphincter, the perineal nerve allows us to control the release of feces, maintaining bowel continence.
Damage or disorders affecting the perineal nerve can potentially result in a loss of motor control, leading to urinary or fecal incontinence. Individuals with perineal nerve dysfunction may experience difficulty in controlling the release of urine or feces, leading to embarrassing and inconvenient situations.
In conclusion, the perineal nerve plays a crucial role in both sensory and motor functions in the human body. It enables us to perceive sensations in the perineal region and maintain voluntary control over urinary and bowel continence. Understanding the importance of this nerve helps us appreciate the impact of disorders or injuries that affect its function, highlighting the need for proper diagnosis and treatment to restore normal bodily functions.
Disorders Associated with the Perineal Nerve
Disorders involving the perineal nerve can have a significant impact on an individual’s quality of life. Understanding the causes, symptoms, and diagnosis of these disorders is crucial in developing effective treatment strategies.
The perineal nerve, also known as the pudendal nerve, is a major nerve in the pelvis that provides sensation to the perineum, which includes the genitals and the area between the anus and the scrotum or vulva. When this nerve is damaged or compressed, it can lead to a variety of disorders that affect both men and women.
Causes of Perineal Nerve Damage
Perineal nerve damage can occur due to various factors, including trauma, compression, or diseases such as diabetes. Traumatic injuries, such as pelvic fractures or surgical procedures, can lead to direct nerve damage. For example, a fall or a car accident can cause a fracture in the pelvis, which can injure the perineal nerve.
Compression of the nerve can result from prolonged pressure on the perineum, often due to sitting for extended periods or cycling. People who spend long hours sitting at a desk or who engage in activities that put pressure on the perineum, such as cycling or horseback riding, are at a higher risk of developing perineal nerve disorders.
Additionally, certain medical conditions, such as diabetes, can damage the peripheral nerves, including the perineal nerve. Diabetes is a chronic condition that affects the body’s ability to regulate blood sugar levels. Over time, high blood sugar levels can cause damage to the nerves, including those in the perineum.
Symptoms and Diagnosis of Perineal Nerve Disorders
The symptoms of perineal nerve disorders can vary depending on the specific condition and the extent of nerve damage. Common symptoms include pain, numbness, tingling, or weakness in the perineal region. These symptoms may be accompanied by difficulties in urinary or bowel control.
Individuals with perineal nerve disorders may experience pain or discomfort during sexual intercourse, as the perineum is a highly sensitive area involved in sexual function. This can have a significant impact on a person’s sexual well-being and overall quality of life.
It is important to consult with a medical professional for an accurate diagnosis, as other conditions can manifest with similar symptoms. A thorough medical history will be taken to understand the onset and progression of symptoms. A physical examination may also be conducted to assess the perineal region and identify any signs of nerve damage.
In some cases, additional diagnostic methods may be necessary to assess nerve function. This can include imaging studies, such as magnetic resonance imaging (MRI), to visualize the pelvis and identify any structural abnormalities. Nerve conduction studies may also be performed to measure the electrical activity of the perineal nerve and determine the extent of nerve damage.
Early diagnosis and intervention are crucial in managing perineal nerve disorders. Treatment options may include pain management techniques, physical therapy, medications to control symptoms, and in severe cases, surgical interventions to release nerve compression or repair damaged nerves.
Living with a perineal nerve disorder can be challenging, but with proper medical care and support, individuals can manage their symptoms and improve their quality of life. It is important to work closely with healthcare professionals to develop a personalized treatment plan that addresses the specific needs and goals of each individual.
Treatment and Management of Perineal Nerve Disorders
The treatment of perineal nerve disorders aims to alleviate symptoms, improve nerve function, and enhance overall quality of life. It is important to note that treatment approaches may vary depending on the underlying cause and severity of the condition. While this article does not provide medical advice, some general approaches to managing perineal nerve disorders are worth mentioning.
Perineal nerve disorders can cause a variety of symptoms, including pain, numbness, tingling, and weakness in the perineal region. These symptoms can significantly impact daily activities and quality of life. Therefore, effective treatment is essential to restore normal nerve function and alleviate discomfort.
Non-Surgical Treatments for Perineal Nerve Disorders
Non-surgical treatments may include medications to relieve pain or manage underlying medical conditions. Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, can help reduce pain and inflammation associated with perineal nerve disorders. Additionally, medications that target specific underlying conditions, such as antiviral drugs for herpes infections or immunosuppressants for autoimmune disorders, may be prescribed.
Physical therapy exercises targeting the perineal region can also play a crucial role in the management of perineal nerve disorders. These exercises aim to improve muscle strength and control, promoting better overall function. Physical therapists can provide guidance on specific exercises and techniques that can be incorporated into a daily routine.
Lifestyle modifications can complement medical treatments and physical therapy exercises. For example, avoiding prolonged sitting or cycling can help reduce pressure on the perineal region, relieving symptoms. Engaging in regular physical activity, such as walking or swimming, can also promote overall health and well-being.
Alternative therapies, such as acupuncture or nerve stimulation, may be explored in consultation with a healthcare professional. These therapies aim to stimulate nerve function and promote healing. However, it is important to discuss these options with a qualified healthcare provider to ensure their safety and effectiveness.
Surgical Interventions for Perineal Nerve Disorders
In some cases, surgical interventions may be necessary to address specific conditions causing perineal nerve disorders. Surgical options will depend on the underlying cause and may range from nerve decompression to nerve grafting or transfer procedures.
Nerve decompression surgery involves relieving pressure on the affected nerve by removing or repositioning surrounding structures. This can help restore normal nerve function and alleviate symptoms. Nerve grafting or transfer procedures may be performed to repair damaged or severed nerves, allowing for regeneration and improved function.
It is crucial to have a thorough discussion with a qualified surgeon to understand the potential risks, benefits, and expected outcomes of any surgical intervention. The decision to undergo surgery should be based on a careful evaluation of the individual’s specific condition and needs.
In conclusion, the treatment and management of perineal nerve disorders involve a multidisciplinary approach. Non-surgical treatments, such as medications, physical therapy exercises, and lifestyle modifications, can help alleviate symptoms and improve overall function. Surgical interventions may be necessary in certain cases to address the underlying cause of the disorder. Consulting with healthcare professionals and specialists is essential to develop an individualized treatment plan that best suits the patient’s needs and goals.
Future Research Directions in Perineal Nerve Study
The field of perineal nerve study continues to evolve, and future research endeavors hold promise for better understanding, diagnosis, and treatment of associated disorders. Technological advancements and potential therapies are areas of particular interest.
One area of research that shows great potential is the development of advanced medical imaging techniques for studying the perineal nerve. For example, magnetic resonance imaging (MRI) and ultrasound are being explored as tools to enable more precise visualization of the perineal nerve and its surrounding structures. This improved imaging can enhance diagnostic accuracy and aid in surgical planning. Researchers are also investigating the use of advanced imaging techniques to study the functional connectivity of the perineal nerve with other parts of the nervous system, providing valuable insights into its role in various bodily functions.
In addition to imaging advancements, ongoing research in nerve regeneration and tissue engineering may hold promise for novel treatment approaches to restore perineal nerve function. Scientists are exploring regenerative medicine techniques, such as stem cell therapy or nerve tissue grafting, aimed at promoting nerve regeneration and restoring normal function. These cutting-edge therapies have the potential to revolutionize the treatment of perineal nerve disorders, offering hope to patients who currently have limited treatment options.
Another exciting area of research is the development of potential therapies for perineal nerve disorders. Emerging strategies include neuromodulation techniques, such as spinal cord stimulation or peripheral nerve stimulation. These techniques involve the use of electrical impulses to modulate the activity of the perineal nerve, offering a non-invasive and potentially effective approach to manage pain and improve functional outcomes. Researchers are also investigating the use of targeted drug delivery systems to deliver therapeutic agents directly to the perineal nerve, minimizing side effects and maximizing treatment efficacy.
Furthermore, advancements in our understanding of the genetic and molecular basis of perineal nerve disorders are paving the way for personalized medicine approaches. By identifying specific genetic mutations or molecular pathways associated with these disorders, researchers can develop targeted therapies that address the underlying causes, leading to more effective and tailored treatment options.
In conclusion, understanding the distribution of the perineal nerve is crucial to grasp its anatomy, role, associated disorders, and treatment options. This comprehensive overview provides a foundation for further inquiry and highlights the importance of consulting with healthcare professionals for accurate diagnosis and personalized advice. With ongoing research and technological advancements, the future holds promising possibilities for a better understanding and management of perineal nerve disorders. Researchers and healthcare professionals are working tirelessly to unlock the mysteries of the perineal nerve, with the ultimate goal of improving the lives of individuals affected by these disorders.